Trying to have a baby can feel overwhelming, especially when male factor infertility is part of the challenge. You might be wondering: Will IUI work for us? What do these sperm analysis numbers really mean?
If you're exploring IUI as a treatment for male factor infertility, understanding how it works, when it's recommended, and what to expect during the treatment process can help both of you move forward with confidence and clarity.
What is IUI?
Intrauterine insemination (IUI) is a fertility treatment where specially prepared sperm is placed directly into your uterus (womb) around the time of ovulation. This treatment helps increase the number of sperm that reach your fallopian tubes, enhancing your chances of fertilisation, especially when you have concerns about sperm quality.
IUI is less invasive and more affordable than other fertility treatments like IVF (in vitro fertilisation). That’s why it’s usually the first-line treatment your doctor suggests if you’re facing mild to moderate fertility challenges.
What is male factor infertility?
Male factor infertility refers to a problem with a man’s sperm that affects the ability to get pregnant. It’s actually more common than you might think – accounting for roughly 30%–50% of all infertility cases.
Your doctor will diagnose the problem through a semen analysis – a straightforward test that evaluates the concentration (number of sperm), motility (movement), and morphology (shape) of your partner’s sperm.
Common causes of male factor infertility may include:
Low sperm count (oligospermia)
Poor sperm motility (asthenozoospermia)
Abnormal sperm shape (teratozoospermia)
Obstruction or blockage in the reproductive tract
Hormonal imbalances
Varicocele (enlarged veins in the scrotum)
Prior illness, infection, or injury.
If you or your partner are affected by one of these conditions, you’re not alone. With the right treatment, many of these conditions can be identified and accounted for before you begin your fertility journey. Your doctor will work with you to identify the specific cause and explore the right approach for your situation.
Worried that you or your partner might be affected by male factor infertility? Schedule an appointment with Thomson Medical to speak with our fertility specialists who can guide you through the tests and provide advice on your next steps.
Can IUI help with male infertility?
IUI helps by:
Bypassing cervical mucus, which may restrict sperm movement
Delivering concentrated, motile sperm closer to the egg
Enhancing the odds of fertilisation during the fertile window
However, if the sperm count is very low or sperm mobility is limited, your doctor may recommend other treatments that offer a higher chance of success, such as IVF with ICSI (intracytoplasmic sperm injection). If this happens to you, don’t worry; your doctor will talk you through every option so you can make the choice that feels right.
Additional Considerations for Vasectomy
(if you had it before) is still possible with sperm retrieval techniques like TESE (testicular sperm extraction) or PESA (percutaneous epididymal sperm aspiration). These methods allow sperm to be collected for use in procedures like IUI, but your doctor will guide you on the best options for your individual situation.Your doctor will guide you toward the fertility option for your individual situation, so that you understand the likelihood of success and all alternatives available.
What sperm parameters affect IUI success?
Understanding the numbers in your semen analysis might help you and your doctor decide if IUI is right for you.
Here’s what matters most:
Total Motile Sperm Count (TMSC):
This is the number of moving sperm in the ejaculate after sperm processing.
A TMSC of more than 10 million is usually associated with higher IUI success rates, while 5–10 million may still be acceptable and gives reasonable chances.
Below 5 million, the success rate drops significantly. In this case, your doctor might suggest alternative options.
Sperm motility:
This measures the percentage of sperm that are actively moving, especially those swimming forward (called progressive motility).
A motility rate above 32% is usually considered enough for IUI to work.
Sperm morphology:
This refers to how many sperm have a normal shape. According to the strict Kruger criteria, a morphology of 4% or higher is considered normal.
IUI can still be beneficial if your sperm count and motility are within a healthy range, even if your morphology is a little below normal.
While these numbers give your doctor a clearer picture, they’re not the only factors that matter. Your doctor will help guide you through these tests and explain how they can be used to improve your chances with IUI.
Our IUI specialists in Singapore
Loading...
When is IUI recommended for male factor issues?
IUI is a suitable option when your partner is dealing with:
Mild to moderate low sperm count:
Your doctor will look for at least 5 million total motile sperm after processing.
Reduced motility:
Even if motility isn’t perfect, IUI can work as long as there are enough active sperm after preparation.
Mild morphology issues:
If sperm shape is slightly abnormal but your count and motility are within range, IUI is still effective.
Situational issues:
IUI can help overcome difficulty with ejaculation or retrograde ejaculation.
Borderline sperm abnormalities:
If no other causes of infertility have been detected, your doctor will analyse all aspects to determine if IUI is the best first step for you.
Sperm preparation for IUI in male factor infertility
Before your IUI procedure, our doctor will prepare the semen sample through a process called sperm preparation or sperm washing. This step is especially important for male factor infertility because it isolates and concentrates the healthiest and most active sperm.
The two most popular methods your doctor may use are:
Swim-up method:
This technique depends on the sperm’s natural ability to swim upwards into a nutrient-rich medium, allowing your doctor to collect the most active ones.
Density gradient centrifugation:
Your doctor layers the semen over special solutions and spins it in a machine (centrifuge). This separates the sperm by quality, and your doctor will collect the best ones from the bottom layers.
During preparation, your doctor removes dead sperm, debris, white blood cells, and chemicals (prostaglandins) from the semen that could cause uterine cramping or inflammation. The result will be a small sample of the healthiest and most active sperm that is ready for your IUI procedure.
IUI and male infertility: What to expect
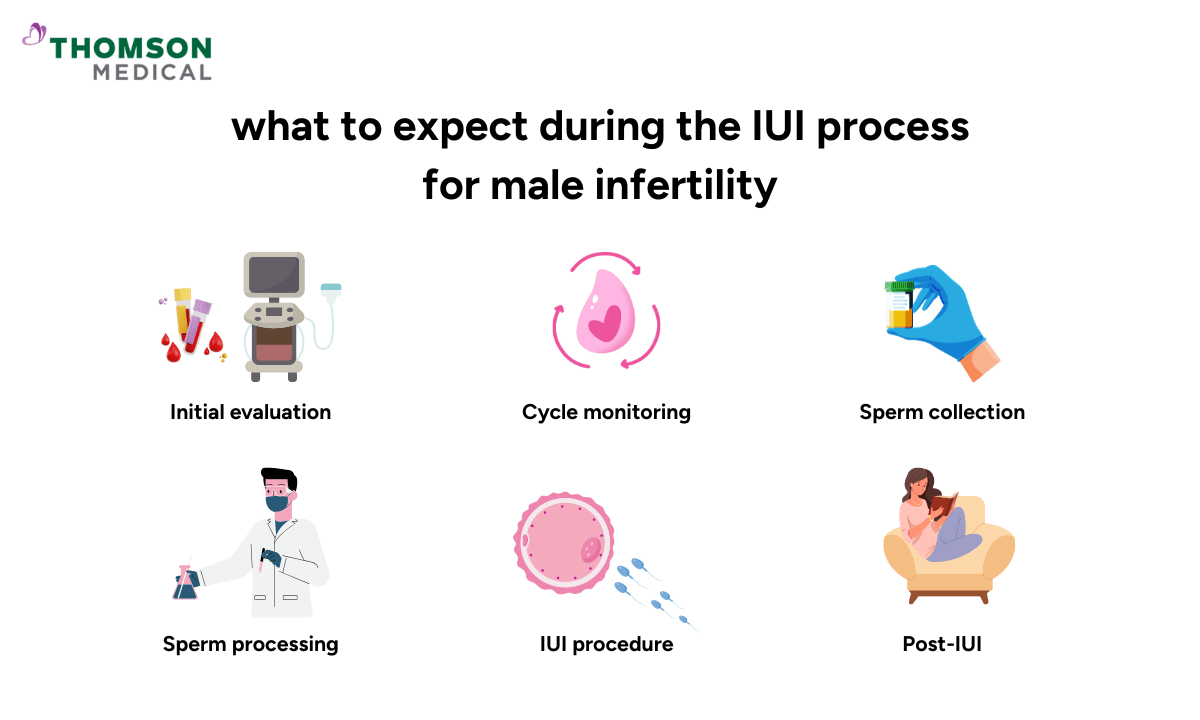
If you and your partner are pursuing IUI due to male factor infertility, here’s what the process looks like:
Initial evaluation:
Your partner undergoes a semen analysis, and your doctor will examine your ovulation and uterine health.
Blood tests, pelvic ultrasounds, and cycle tracking may also be done.
Cycle monitoring:
Your ovulation is tracked with urine LH kits, blood hormone levels, or an ultrasound.
In some cases, you may get medication, such as clomiphene or letrozole, to stimulate ovulation and increase the chances of releasing a healthy egg.
Sperm collection:
On the day of the IUI procedure, your partner will provide a semen sample through masturbation after 2–5 days of abstinence. Your doctor will ensure your partner’s privacy during the process.
If you use frozen or donated sperm, the sample is thawed and prepared in the lab.
Sperm processing:
Your fertility specialist will wash and concentrate the sample to get the healthiest sperm.
IUI procedure:
Your doctor inserts a small and flexible tube into your uterus and injects the prepared sperm.
The procedure takes about 5–10 minutes, and you won't need anaesthesia. It's usually painless, though you might feel a bit of pressure or discomfort. After that, your doctor may ask you to rest before leaving.
Post-IUI:
You can go back to your normal activities right away. A pregnancy test is usually done 14 days later to determine if the cycle was successful.
It's completely normal to feel anxious during the two-week wait. Remember, you don’t need to go through this experience alone. Your doctor understands and is always available whenever you need support.
If you have any concerns about the procedure, don't hesitate to talk to your doctor. They'll make sure all your questions are answered and that you feel comfortable moving forward.
If you're concerned about male factor infertility or wondering whether IUI is right for you, schedule an appointment with Thomson Medical. Our fertility specialists will assess your specific situation, discuss your options, and create a personalised treatment plan that can help improve your chance of success.
FAQ
Is IUI effective for male factor infertility and low sperm count?
Yes, IUI can be effective for mild to moderate male factor infertility. When the sperm count, motility, or morphology is slightly below normal, the IUI procedure can improve the chances of pregnancy by delivering sperm directly into your uterus. This bypasses cervical mucus and reduces the distance sperm need to travel to reach your egg.
For low sperm count, especially when the total motile sperm count after sperm washing is at least 5-10 million, success rates are still reasonable, approximately 10-15% per cycle. When sperm count is very low (less than 5 million post-wash), the success rates of IUI drop significantly.
However, IUI is less effective for severe male infertility, such as very low sperm counts or poor motility. In such cases, IVF with ICSI may be a better option for you and your partner because it allows for the direct injection of a single healthy sperm into your egg.
It’s natural to feel overwhelmed when learning about these treatments. Your doctor will assess your partner’s and your conditions and answer all of the concerns you might have to help you choose the right approach.
What is the success rate of IUI for male factor infertility?
IUI success rates for male factor infertility vary based on the severity of sperm issues but usually range from 10% to 15% per cycle for mild to moderate male infertility.
Most couples try 3–6 cycles before getting pregnant. Your doctor will review your semen analysis results and other fertility factors before creating a personalised estimate for you.
Is IUI or IVF better for male infertility?
IUI works best for mild to moderate sperm issues, when there are more than 5 million motile sperm after processing. This treatment is also less invasive and more affordable than IVF.
IVF with ICSI is preferable for severe sperm problems, when there are fewer than 5 million motile sperm, or if you have tried IUI cycles without success.
Your doctor will help you decide which treatment gives you the highest chance based on your tests and overall fertility picture.
What is the best treatment for male factor infertility?
It depends on what's causing the problem and how severe it is. Your doctor will work with you to find the best solution, which might include:
Lifestyle changes:
Losing weight, quitting smoking, reducing alcohol, and treating infections can improve sperm quality.
Medications:
Hormonal therapy can help if you have low testosterone or issues with your pituitary dysfunction
IUI:
It’s a good first step for mild male infertility
IVF with ICSI:
Your doctor may recommend it for moderate to severe sperm abnormalities
Surgical interventions:
It helps you overcome varicoceles or ejaculatory duct obstruction
Donor sperm:
It can be an option if no viable sperm is present, giving you and your partner a chance to become parents.
Can male factor infertility be cured?
In some circumstances, yes. Male infertility can be treated or reversed, depending on the cause. For example:
Varicocele repair:
It may help improve sperm quality and count
Hormonal imbalances:
Hormonal problems can usually be treated with medication
Infections:
Antibiotics can treat bacterial infections
Lifestyle changes:
Having a healthy lifestyle can increase fertility in men with lifestyle-related sperm issues
However, in cases of genetic defects, testicular failure, or permanent damage to the reproductive organs, infertility may not be curable. In these situations, assisted reproductive technologies (ART) or the use of donor sperm may be the better options for you.
Is donor sperm recommended for severe male factor infertility?
Yes, your doctor may recommend donor sperm when male infertility is severe and other treatments haven’t worked. This might include:
No sperm production, especially if non-obstructive (azoospermia)
Severely abnormal sperm that cannot be used, even with ICSI
Genetic disorders that could be passed to offspring
Multiple unsuccessful IVF/ICSI cycles.
Using donor sperm is a deeply personal decision, and it’s completely normal to have mixed feelings about it. Your doctor will only discuss this option after you have been through tests and tried other options first. If using your partner's sperm isn't possible or advisable, donor sperm can open a real path to parenthood.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice based on your unique situations, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
For more information, contact us:
Thomson Fertility
- Paragon: 6252 7766
Thomson Specialists (Women's Health)
Request an Appointment