Ovarian cancer is often difficult to detect early, which is why many women only start learning about it after symptoms appear. This can feel worrying, especially if you are unsure whether you may be at risk.
Factors such as genetics, family history, and the type of birth control you used in the past can all influence your chances of being diagnosed with ovarian cancer. Some of these are beyond your control, while others may offer opportunities to manage your risk.
Understanding your ovarian cancer risk factors can help you have meaningful conversations with your doctor, make informed health decisions, and spot any warning signs before they grow into serious issues.
What is ovarian cancer?
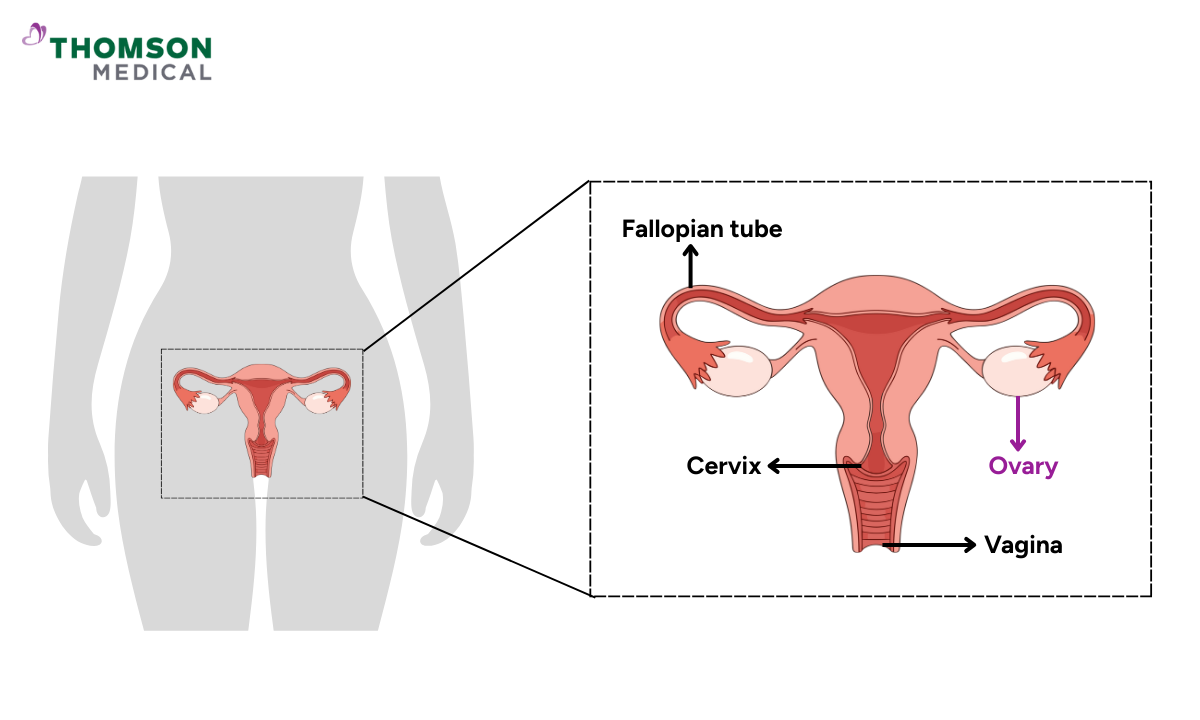
Ovarian cancer happens when abnormal cells in your ovaries grow out of control. Your ovaries are part of your reproductive system, located on either side of your uterus in your lower abdomen. They produce eggs and hormones like oestrogen and progesterone that support your menstrual cycle.
Early-stage ovarian cancer rarely causes obvious symptoms, which is why it can spread to nearby organs before being detected. That's why it's worth understanding your cancer risk and knowing what early symptoms to look for. Finding cancer early can genuinely make all the difference to your treatment and outcome.
Who is at high risk for ovarian cancer?
Anyone with ovaries can develop ovarian cancer, but your individual risk depends on several factors. Many women worry about having a higher risk, especially as they get older or if cancer runs in their family.
Most cases occur in women over 50, with the average age at diagnosis being around 63. However, certain factors can increase your risk at any age. Knowing what increases your risk helps you look after yourself better. By spotting symptoms earlier and making changes that could genuinely reduce your chances of developing the disease.
What factors increase your risk?
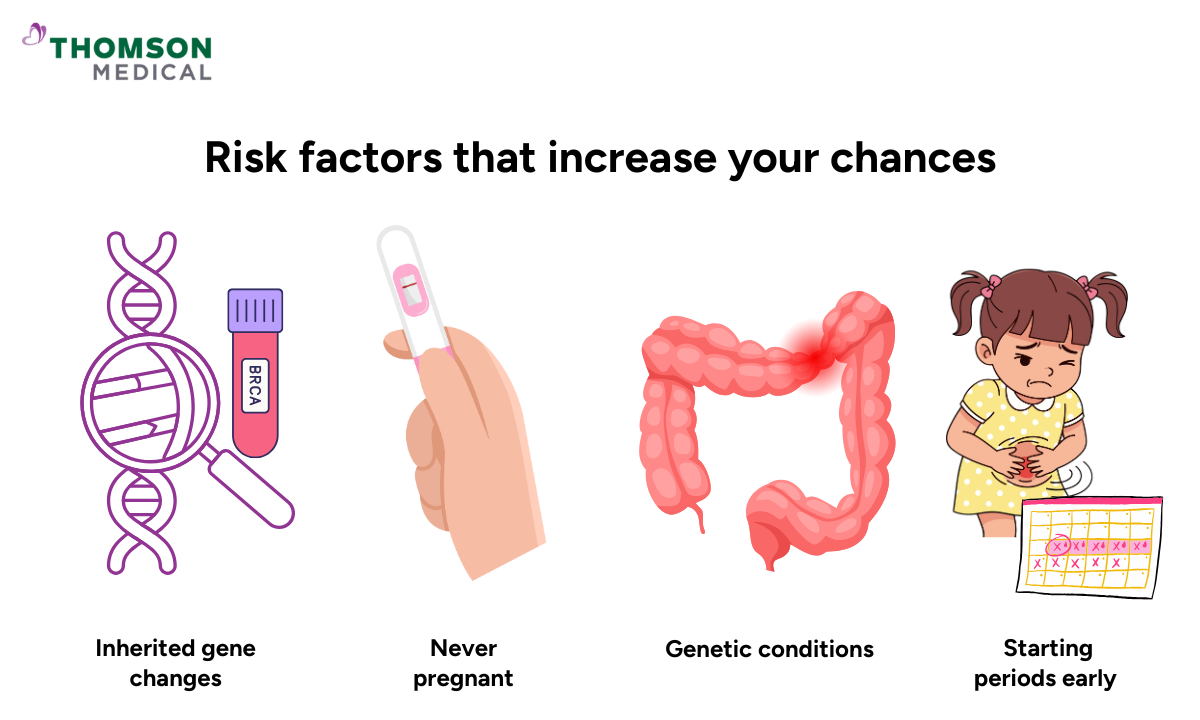
Several factors may raise your chances of developing ovarian cancer. These include:
Family history of ovarian, breast or colorectal cancer
Never having been pregnant
Inherited gene changes, especially BRCA 1 or BRCA 2 mutations
Starting periods early or experiencing menopause late
Long-term use of hormone replacement therapy
Genetic conditions like Lynch syndrome
It's important to remember that while these factors do increase your risk, many women with them never develop ovarian cancer. Having one or more risk factors doesn't mean you'll definitely get the disease – it means paying closer attention to any unusual symptoms and letting your doctor know so they can advise on prevention.
Ovarian cancer specialists
Loading...
What can lower your risk?
You cannot completely prevent ovarian cancer, but there are ways that may help lower your risk:
Using birth control pills (called oral contraceptives)
Pregnancy and breastfeeding
Healthy lifestyle choices, including balanced nutrition, avoid smoking and regular physical activity
These are just a few simple steps you can take to reduce your ovarian cancer risk. Birth control pills, pregnancy and breastfeeding naturally change your hormone levels in ways that may offer protection. Healthy lifestyle habits support your body's overall health and wellbeing.
While there's no guaranteed way to prevent ovarian cancer, these choices can help reduce your risk and support your long-term health.
What can you do if you're at higher risk?
If you have a strong family history of ovarian or breast cancer, or you know you carry genetic mutations, you can work with your doctor on preventive steps.
This might involve:
Genetic counselling and genetic testing to understand your specific risk
Regular medical checkups with your doctor or a specialist
Certain surgical procedures like removal of ovaries or fallopian tubes (only for medical reasons in higher-risk situations)
Decisions about surgical procedures are personal and should be made together with your doctor. They'll consider your age, overall health, fertility plan, and the specifics of your case. You don't need to rush this decision. Your doctor will explain your options and help you choose what's right for your situation.
If you’re concerned about your ovarian cancer risk, request an appointment with Thomson Medical to discuss genetic counselling, testing, and appropriate monitoring. Our doctors can review your personal and family history and help you decide on the next steps that are right for you.
Can ovarian cancer be detected early?
Unlike cervical screening or breast mammograms, there's no reliable screening test that can catch it early in most women. Most cases are found when women notice persistent symptoms and see their doctor.
If you're at higher risk due to genetic mutations, your doctor may recommend regularly monitoring your pelvic area through pelvic exams, transvaginal ultrasound, or blood tests like CA-125. These tests aren't used for routine screening, but they can help investigate symptoms or keep a closer watch if you're in a higher-risk group.
The most important thing you can do is know which symptoms to watch for and check yourself if something doesn't feel right. Don't dismiss changes that persist for more than two weeks.
When should you see a doctor?
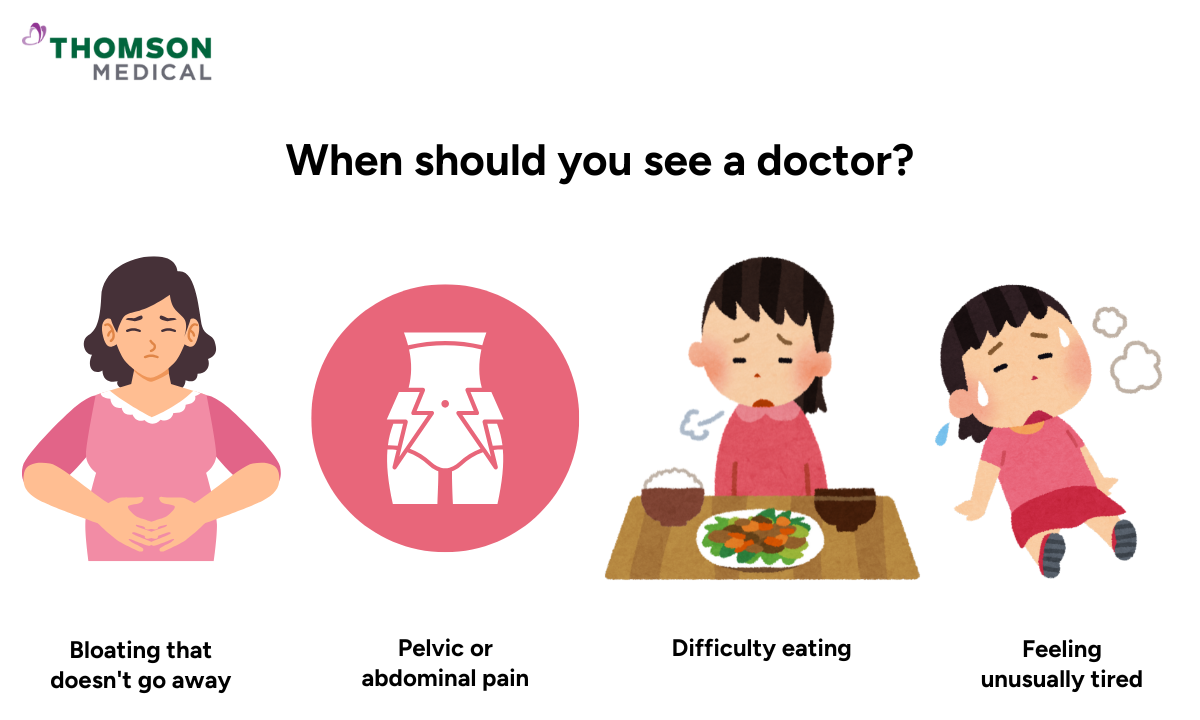
Early symptoms of ovarian cancer are often vague and easily mistaken for minor digestive issues. But if you experience any of these for several weeks, you should consider getting yourself checked just in case:
Bloating that doesn't go away
Pelvic or abdominal pain
Difficulty eating or feeling full quickly (early satiety)
Needing to urinate more frequently
Feeling unusually tired
If you're experiencing any of them, see your doctor. It's important to remember that these symptoms are far more commonly caused by other, less serious conditions. Catching any health issue early, whether it's cancer or something else, means you can get the right treatment sooner.
Persistent symptoms deserve proper assessment. Request an appointment with Thomson Medical to discuss ongoing bloating, pelvic pain, or changes in appetite or urination so your doctor can investigate early and advise on the next steps.
FAQ
How can you find out if you are at high genetic risk?
Genetic counselling and genetic testing can help determine if you carry gene changes like BRCA 1 or BRCA 2. This is particularly important if close family members have had ovarian or breast cancer. Your doctor can refer you to a genetic counsellor who will assess your family history.
Can lifestyle choices influence your risk?
Yes, though lifestyle isn't the whole story. Healthy habits like regular physical activity, maintaining a healthy weight, and not smoking may help lower your overall cancer risk. These choices support your wellbeing even if they can't guarantee prevention.
What causes ovarian cancer?
There isn't a single cause. Most cases of ovarian cancer develop due to a combination of factors, including genetics, age, and changes in cells over time. For many women, the exact cause remains unknown.
How can ovarian cancer be detected early?
Early detection relies mainly on recognising persistent symptoms of ovarian cancer and seeking medical attention. There's no routine screening test available. If you notice bloating, pelvic pain, eating difficulties, or frequent urination lasting several weeks, see your doctor.
How can ovarian cancer be prevented from coming back?
After the treatment, follow your doctor's recommended care plan and attend regular appointments. Maintain healthy lifestyle habits and report any new or unusual symptoms promptly. Your medical team will monitor you closely.
How long can you have ovarian cancer without knowing?
Ovarian cancer can sometimes develop over months or even years without causing obvious symptoms. This is why it's often diagnosed at a later stage. Pay attention to persistent changes in your body and discuss them with your doctor.
Should everyone consider genetic testing?
Not necessarily. Genetic testing is most useful for people with a strong family history of ovarian cancer, breast cancer, or related colorectal cancer. If several close relatives have had these cancers, especially at younger ages, speak with your doctor about whether genetic counselling would be helpful.
The information is intended for general guidance only and should not be considered medical advice. For personalised recommendations and advice based on your unique situation, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) - Jurong:
6262 8588 (Call), 6262 8588 (WA) - Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
Notice
The range of services may vary between TWC/TS locations. Please contact your preferred branch directly to enquire about the current availability.
Request an Appointment