If you’ve just received a stage 1 cervical cancer diagnosis, it's understandable to experience feelings of worry and uncertainty. You might be asking yourself questions like, 'How serious is this?' or 'What happens next?'
The encouraging news is that most women with stage 1 cervical cancer respond really well to treatment and go on to be completely cancer-free. Learning your diagnosis is the first step in taking control of what comes next.
What is stage 1 cervical cancer?
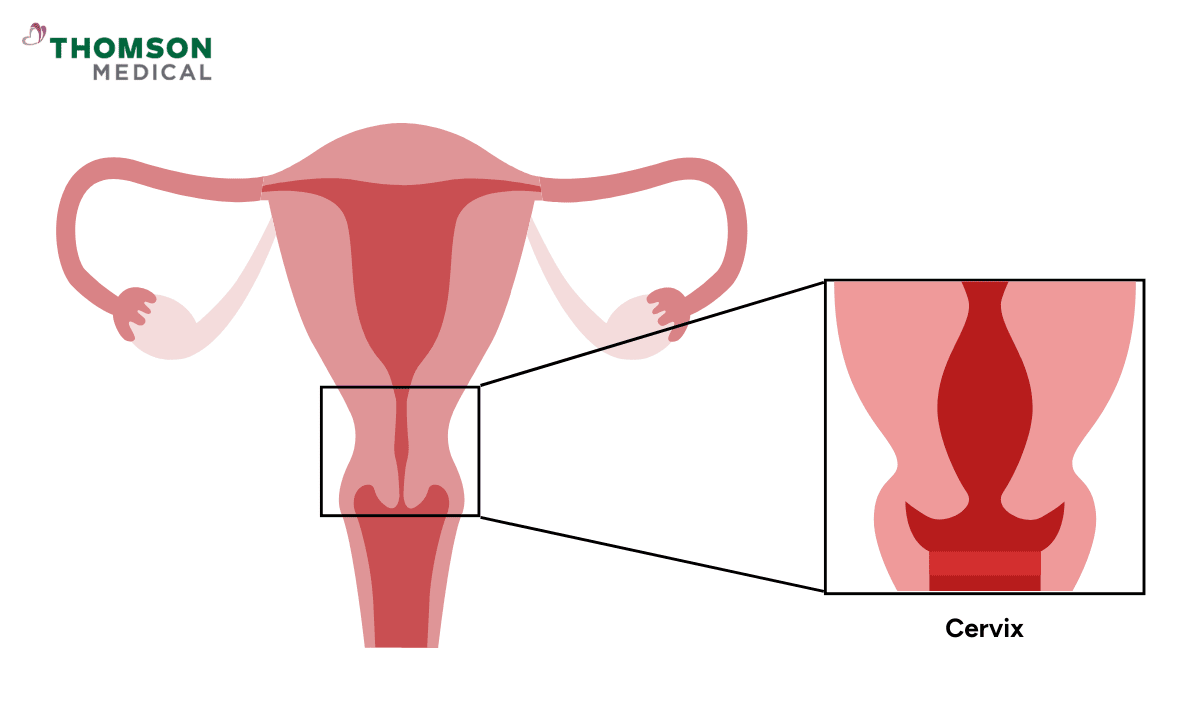
When cervical cancer is caught at stage 1, there is good reason for hope. The cancer is contained only in your cervix and hasn't spread to other parts of your body. This early detection means you have effective treatment options available.
When the doctor diagnoses "stage 1", it means the cancer is only in your cervix and hasn't spread to other parts of your body.
Doctors divide stage 1 into smaller categories (1A and 1B) based on how large the area is and how deeply it has grown into your cervical tissue.
Stage 1A (the earliest stage)
This is the very beginning of cervical cancer. It's so tiny that your doctor can only see it under a microscope.
Stage 1A1:
The cancer has grown 3 mm or less in your cervical tissue. To help you picture this, imagine the thickness of two 50-cent coins stacked.
Stage 1A2:
The cancer has grown a bit deeper, between 3 mm and 5 mm.
Stage 1B
At this stage, the tumor is larger but remains confined only to the cervix. This means it hasn't reached nearby organs or lymph nodes.
Stage 1B1:
The area is 2 cm or smaller (about the size of a grape) and has grown deeper than 5 mm.
Stage 1B2:
The area is between 2 cm and 4 cm (roughly the size of a walnut).
Stage 1B3:
The area is larger than 4 cm.
Fortunately, stage 1 cervical cancer is still considered an early stage, meaning that treatment during this phase has a very high success rate. Most women recover well and stay cancer-free after treatment.
What symptoms might you notice?
The early symptoms of cervical cancer can be very subtle, and you might not notice anything unusual at first. Many women with stage 1 cervical cancer don't notice any symptoms at all, which is why the cancer is often found during routine screening rather than because something felt wrong.
That said, you might experience things like:
Unusual vaginal bleeding between periods, after sexual contact, or after menopause
Vaginal discharge that seems different than usual, perhaps watery or with an unusual smell
Pelvic pain or in lower back pain
Feeling more tired than usual or losing weight without trying
Discomfort when you pass urine
These symptoms can happen for many reasons that aren't related to cancer. If you've been experiencing any of them, it's a good idea to check with a medical professional who can identify the cause and advise you on the best course of action.
Our cervical cancer specialist
Loading...
How is stage 1 cervical cancer diagnosed?
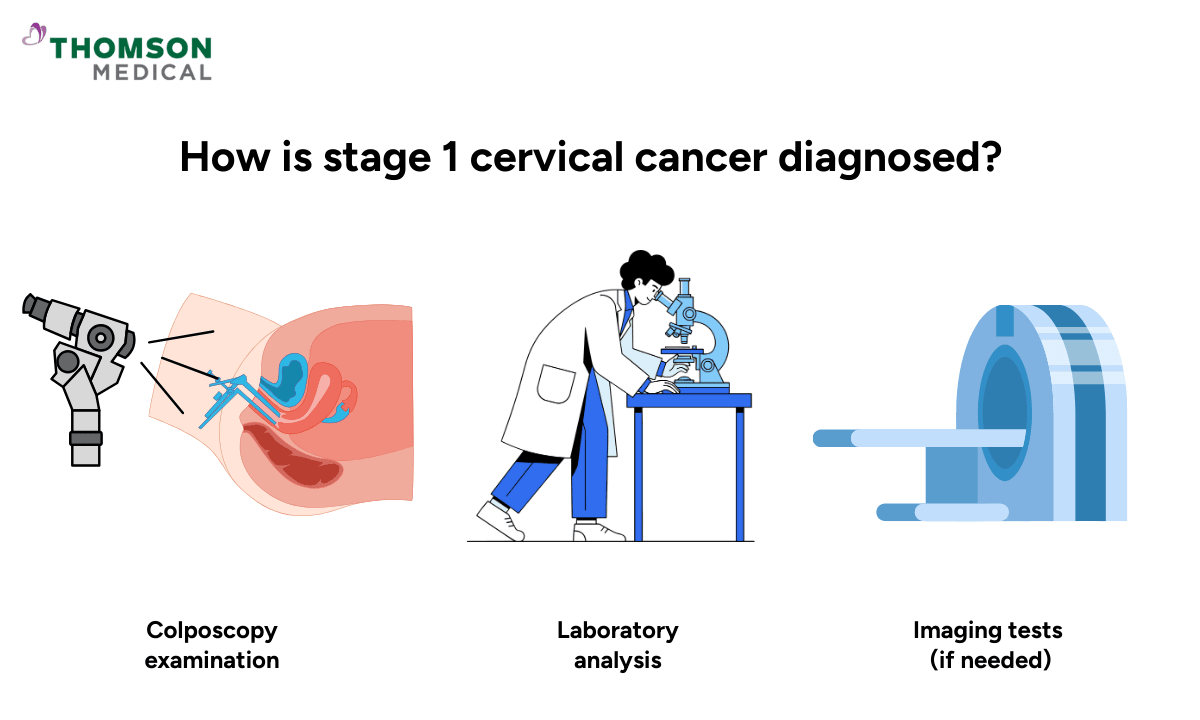
For most women, cervical cancer is first detected during routine screening. It's completely normal to feel anxious or uncertain when undergoing these tests, but they are designed to catch problems early when they're most treatable. The process typically involves:
Initial detection through routine screening:
Colposcopy examination:
Your doctor uses a special magnifying tool to look at your cervix more closely.
If something looks unusual, they'll take a small tissue sample called a biopsy. This might sound scary, but it's a quick procedure.
Laboratory analysis:
The biopsy helps confirm whether cancerous cells are present and what type they are.
The most common type is called squamous cell carcinoma, which starts in the cells on the outer part of your cervix.
Imaging tests (if needed):
Your doctor might suggest scans like a CT or MRI to get a clearer picture of the size and to check nearby areas.
Going through all these tests can feel like a lot. But having clear, detailed information means your doctor can create the most effective treatment plan specifically for you.
What are your treatment options?
It’s normal to feel anxious when thinking about the treatment you’ll need. Everyone’s cancer experience is unique, and your treatment will depend mainly on how large the area is and how deep it has grown. Here are the main types of surgery for stage 1 cervical cancer:
Type of surgery | What it involves | Best for |
Removes a cone-shaped piece of your cervix | Very early cancers (1A1) that preserve fertility | |
Radical trachelectomy | Removes your cervix and some nearby tissue but keeps your uterus (womb) | Small tumours that may preserve fertility |
Total hysterectomy | Removes your uterus and cervix | Larger tumours or if you don't plan more children |
For most women with stage 1 cervical cancer, surgery alone works very well. In some cases, your doctor may suggest adding chemotherapy with radiation after surgery. This combination is recommended to give you the best possible chance of staying healthy and cancer-free.
What are your chances of recovery?
This is probably one of the first questions on your mind, and wanting to understand your chances of recovery is an important part of your journey.
The chances for stage 1 cervical cancer are genuinely very positive. Around 90–95% of women diagnosed with early-stage cervical cancer are alive and well five years later, and many are living completely cancer-free lives.
Your recovery chances will depend on your specific substage, how large the area is, and your overall health. What really matters is that finding the cancer at stage 1 means you're starting from a strong position.
If you've been diagnosed with stage 1 cervical cancer or are concerned about your risk factors, request an appointment with Thomson Medical. Our specialist can guide you through treatment options that prioritise both high survival rates and maintaining your quality of life throughout recovery.
What does life look like after treatment?
Once your treatment is completed, your care continues with regular follow-up appointments. Your doctor will stay connected with you to monitor your recovery and overall health.
During the first two years, you'll typically come in for checkups every 3–4 months. After that, appointments are usually spread out every 6–12 months for another 3 years and then once a year.
These visits are a chance for your doctor to check in on how you're doing. They might include a physical exam, a Pap test, or other tests as needed.
You might have some physical discomfort, notice changes in your intimate life, or have concerns about urination. If you're experiencing any of these issues, please don't hesitate to bring them up with your doctor, as they can suggest treatments to help you feel more comfortable and maintain your quality of life.
How does treatment affect fertility?

If you haven't had children yet, or if you're hoping to have more, you're probably wondering how treatment will affect this part of your life. If this is an important matter for you, please discuss it with your doctor before treatment begins. Your fertility goals are an important part of planning the right treatment approach for you.
Fertility-sparing options
For women with very early-stage cervical cancer (especially stages 1A1 to 1B1) who have small, low-risk tumours, fertility-preserving procedures may be possible.
Cervical conisation or simple trachelectomy:
Removes your cervical tissue that contains the cancer cells while keeping your uterus, giving you the best chance for natural conception later.
Radical trachelectomy:
Removes your cervix and some surrounding tissue but preserves your uterus and ovaries.
Chemotherapy followed by less extensive surgery:
If your tumour is larger (2 cm or more), chemotherapy may reduce its size first, allowing for a more conservative surgical approach.
What about pregnancy after surgery?
If you do become pregnant after surgery, your pregnancy will be monitored more closely than usual, as there's a slightly higher chance of miscarriage or earlier delivery. But don’t worry. Many women go on to have healthy pregnancies and babies with the right medical support.
If your treatment affects your ability to carry a pregnancy, you can look into fertility-preserving techniques such as freezing eggs or embryos before treatment. Your doctor can guide you through these choices and help you decide what’s best for you.
When can you try to conceive?
Most doctors recommend waiting 6 months to 2 years after treatment before trying to get pregnant. This gives your body time to heal and lets your doctor keep an eye on your recovery. Your exact timeline will depend on your treatment and how you’re healing.
Getting your periods back is a positive sign, but your body may still need time before trying to conceive. Talk to your doctor about the best timing for you and explore what options are available based on your individual situation.
If you're concerned about fertility after cervical cancer treatment, request an appointment with Thomson Medical. Our specialist will review your treatment options, discuss fertility-sparing procedures, and provide personalised guidance on safely planning a future pregnancy.
FAQ
Can stage 1 cervical cancer be cured?
Yes, about 95% of women diagnosed at stage 1 are successfully treated. Because the cancer hasn't spread beyond your cervix, treatment can often remove it completely.
Most women go on to live full, healthy lives afterward. Your personal outcome depends on your specific situation, but the statistics are very much in your favour.
Does stage 1 cervical cancer come back?
Recurrence is quite uncommon. About 95% of women with stage 1A remain cancer-free 10 years after treatment. Your individual risk depends on factors like how deeply the cancer has grown. Your follow-up appointments are designed to catch any changes early, when they're most responsive to treatment.
How long does cervical cancer treatment take?
If you're having surgery, the procedure itself usually takes a few hours. You'll typically stay in the hospital for a few days afterward, then continue recovering at home over several weeks. If radiation therapy is part of your treatment plan, sessions usually run for 5 to 7 weeks and you might have a few additional internal radiation treatments as well.
Can you get pregnant after cervical cancer treatment?
This depends on which treatment you have. Procedures like cone biopsy or radical trachelectomy are designed to preserve your fertility. Hysterectomy or pelvic radiation will prevent pregnancy.
It's really important to speak with your care team about your family planning hopes before treatment starts so they can consider approaches that preserve fertility if they're safe and appropriate for your situation.
Does stage 1 cervical cancer require chemotherapy?
Most women with stage 1 cervical cancer only need surgery. However, in some situations, your doctor might recommend adding chemotherapy along with radiation.
This might be the case if cancerous cells are found in lymph nodes after surgery or if there's significant involvement of tissue around the uterus. When this combination is suggested, it's to help reduce the chance of the cancer coming back.
What's the difference between stage 1A and 1B?
The main difference is size. Stage 1A is microscopic, meaning it can only be detected under a microscope, and it has grown 5 mm or less into your cervical tissue. Stage 1B is larger, visible without magnification, and has grown more deeply into your cervix.
How fast does stage 1 cervical cancer progress?
Cervical cancer typically develops quite gradually over several years. It starts with abnormal cell changes that slowly progress over time. Even at stage 1, these cancers tend to grow relatively slowly, though the pace can vary from person to person.
This gradual development is exactly why regular screenings are so valuable. They can catch changes through early detection, often before cancer has even fully developed.
The information is intended for general guidance only and should not be considered medical advice. For personalised recommendations and advice based on your unique situation, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
References:
Guimarães, Y. M., Godoy, L. R., Longatto-Filho, A., & Reis, R. D. (2022). Management of Early-Stage Cervical Cancer: A Literature Review. Cancers, 14(3), 575. https://doi.org/10.3390/cancers14030575
Salman, L., & Covens, A. (2024). Fertility Preservation in Cervical Cancer—Treatment Strategies and Indications. Current Oncology, 31(1), 296–306. https://doi.org/10.3390/curroncol31010019
For more information, contact us:
Thomson Fertility Centre
- Paragon: 6252 7766
Thomson Specialists (Women's Health)
Thomson Women's Clinic
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
