If you've recently been diagnosed with stage 2 cervical cancer, or you're waiting for test results after an abnormal Pap smear, you're likely feeling a mix of emotions right now. Those feelings are completely valid, and many women in your position have felt exactly the same way.
Understanding what this diagnosis means – and the treatments available – can help make things feel a little less overwhelming. While stage 2 is more advanced than stage 1, it's still very treatable, and many women go on to live healthy, full lives after treatment.
What is stage 2 cervical cancer?
In stage 2, the cancer has grown beyond the cervix into nearby tissues, but it's still within your pelvic area. Most cervical cancers begin in the flat cells on the cervix's surface – doctors call this squamous cell carcinoma. Since this is the most common type, your doctor will have treated many cases like yours.
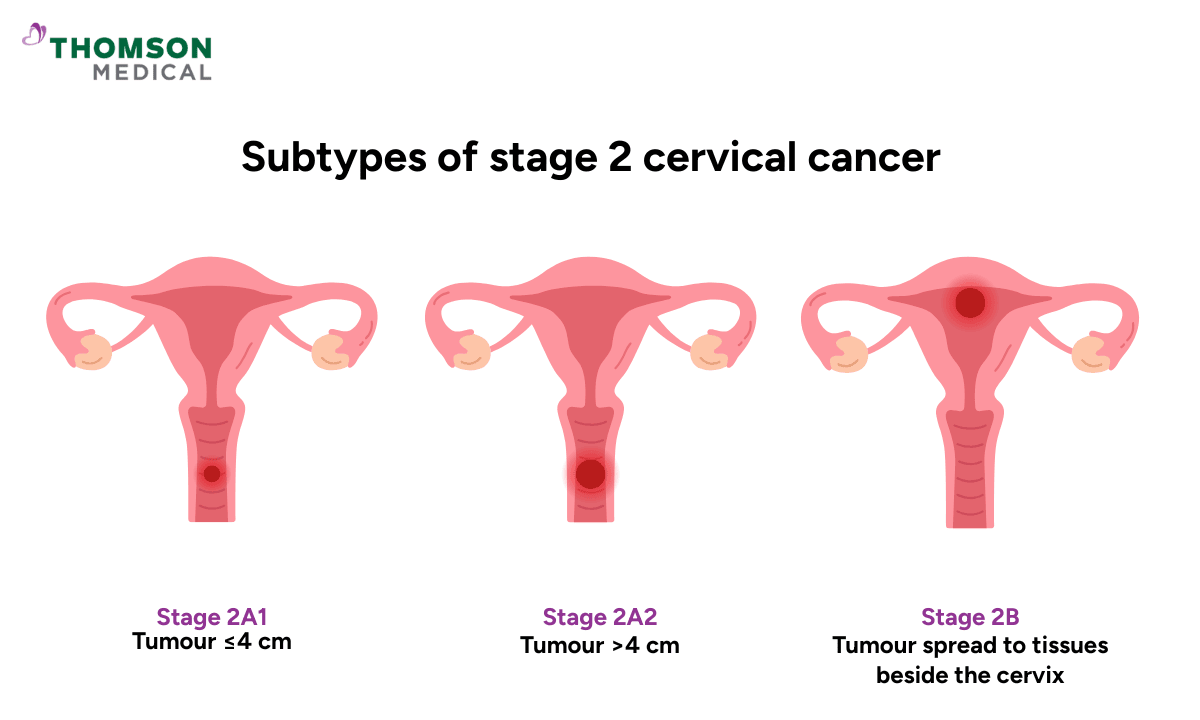
Your doctor might mention terms like 'stage 2A' or '2B' during appointments.
Stage 2A means the cancer has grown into the upper part of your vagina, without reaching the tissues surrounding your uterus.
If the tumor is 4 cm or smaller (about the size of a walnut), it's called 2A1
If it's larger than 4 cm, it's called 2A2
Stage 2B means the cancer has grown into the tissue surrounding your uterus, though it hasn't reached the pelvic wall yet (that's the outer edge of your pelvis). In some cases, nearby lymph nodes may be affected too.
Getting a stage 2 cervical cancer diagnosis can feel overwhelming – that's completely normal. The specifics of your diagnosis matter because they help your doctors create the best possible treatment plan tailored to you.
Our cervical cancer specialist
Loading...
What symptoms of cervical cancer might you notice?
Whatever symptoms brought you to your doctor, it's understandable if they caused you concern. Common signs include:
Abnormal vaginal bleeding after sexual intercourse, between periods, or after menopause
Periods that are heavier or last longer than usual
Unusual vaginal discharge that's watery or has an unpleasant smell
Pain in your pelvis, lower back, or during sex
Unexplained tiredness or weight loss
Some women don't notice any symptoms at all, which is why regular Pap smears and HPV testing are so important for catching changes early – even if you’re feeling perfectly normal.
How did your doctor figure out the cervical cancer stage?
Your doctor will do several tests to get a complete picture of what's happening. While it might feel overwhelming to go through so many tests, each one plays a part in helping your doctor understand exactly what your body needs.
You'll likely have:
A close examination of your cervix using a special magnifying tool called a colposcope. Your doctor can see details that aren't visible to the naked eye.
A biopsy, where a tiny piece of tissue is removed and checked under a microscope. This confirms the cancer and tells your doctor more about it.
MRI or CT scans to see the size of the tumour and whether it's grown into nearby areas. Think of these like detailed photographs that show what's happening inside your body.
A PET scan to check if cancer cells have reached lymph nodes in your pelvis.
In some cases, doctors will check your bladder or bowel to make sure the cancer hasn't affected these areas.
If you have questions about your cervical cancer diagnosis, how your individual risk factors influence your health, or how the staging system affects treatment decisions, request an appointment with Thomson Medical. Our specialist will review your results carefully and guide you through each step of your care.
Treatment options for stage 2 cervical cancer

Your treatment will be designed specifically for you. Your doctors will consider your specific situation, including factors such as whether you have 2A or 2B, the size of the tumour, your overall health, and whether you hope to have children someday.
Facing treatment can bring up a lot of emotions – fear, uncertainty, maybe even grief about the changes ahead. These feelings are valid, and you don't have to face them alone.
Radiation therapy and chemotherapy as primary treatment
If you have stage 2 cervical cancer, especially stage 2B, your doctors will most likely recommend radiation therapy combined with chemotherapy at the same time.
Radiation therapy comes in two forms, and you'll usually have both:
External radiotherapy is given from outside your body.
Internal radiotherapy (also called brachytherapy) delivers radiation from inside your body. A small device is placed inside your vagina, close to where the cancer is, allowing the radiation to target the tumour very precisely.
The chemotherapy works alongside the radiation therapy to target the cancer cells in your body. This combination targets both the tumour you can see and microscopic cancer cells that you can't, preserves your pelvic organs, and reduces the chances of the cancer coming back.
Treatment sessions typically last 5–6 weeks, and it’s completely normal to feel nervous about what to expect. The physical side effects are one thing, but the emotional weight of going through treatment is real too. Your medical team will guide you through each step and help manage any side effects along the way.
When surgery is an option
If you have stage 2A1 (a smaller tumour), surgery might be possible. The surgery is called a radical hysterectomy. This means your surgeon would remove your uterus, cervix, and the tissue around them, along with some nearby lymph nodes to check for cancer cells.
Hearing about this surgery can be overwhelming, and it's normal to feel strongly about its impact on your body and future.
If having children in the future is important to you, speak to your doctor as early as possible – you may still be able to explore options such as egg or embryo freezing before treatment begins.
Even after surgery, your doctor might suggest adjuvant therapy (additional radiation or chemotherapy) to make sure any remaining cancer cells are eliminated. The thought of more treatment after surgery can feel exhausting, but it's there to give you the best chance at staying cancer-free.
What are the survival rates of stage 2 cervical cancer?
You're probably wondering what happens next – and that's one of the hardest parts of a cancer diagnosis. About 60–75% with stage 2 cervical cancer are alive and doing well five years after diagnosis. These numbers can feel intimidating at first, but they come with an important message: many women respond well to treatment and go on to live healthy, fulfilling lives.
Your doctor will monitor you closely after treatment, watching for any signs that the cervical cancer might return and helping you maintain the best possible quality of life.
If you are seeking clarity on overall survival and the impact of cervical cancer on your life, request an appointment with Thomson Medical. Our specialist will guide you through treatment options and long-term monitoring to maintain your health.
Managing side effects and recovery after cervical cancer treatment
Your cervical cancer treatment can affect you both physically and emotionally, and knowing what to expect may help the journey feel a little more manageable.
Side effects of cervical cancer treatment
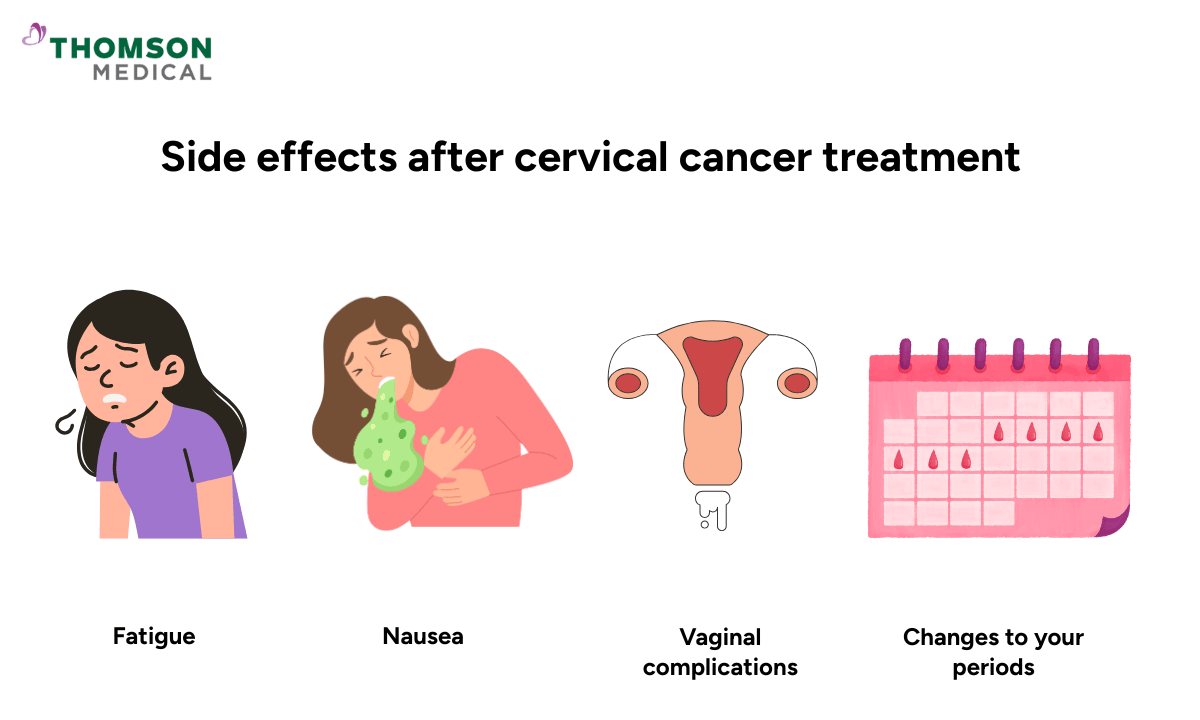
Your body might react in different ways during treatment. Here are some common side effects that you may experience:
Fatigue:
You'll feel tired in a way that sleep doesn't always fix.
Rest when you need to, but try to move gently when you can; even a short walk can help.
Eat nourishing foods when you have an appetite.
Nausea:
The nausea from chemotherapy can be managed with anti-nausea medication from your doctor.
Try eating smaller meals throughout the day instead of three big ones.
Vaginal complications:
Vaginal dryness or discomfort can happen.
Vaginal lubricants and moisturisers can help, and pelvic floor physiotherapy can make a real difference.
Urinary side effects or bowel irritation:
Radiation therapy can lead to bathroom issues.
Drinking lots of water and eating more fibre can help.
Changes to your periods or early menopause:
If the radiation affects your ovaries, you might go through menopause earlier than expected.
Hormone therapy might help, and talking to a counsellor about these changes can make them easier to handle.
Please remember that your doctor is there to help you manage these effects. Don't try to tough it out alone. In this type of situation, it’s important to speak up if something's bothering you, even if it seems small.
Taking care of your emotional health
Cervical cancer doesn't just affect your body. It affects your mind and emotions too.
Many women find these things helpful:
Joining a support group where you can talk to other women who understand what you're going through
Connecting with cancer survivors who've been where you are now
Trying relaxation techniques like meditation, deep breathing, or journaling
Talking openly with your medical team about your worries and fears
Letting your family and friends support you
It's completely normal to feel sad, angry, frustrated, or overwhelmed during treatment. What matters is finding support that works for you, even on the hardest days.
FAQ
Can stage 2 cervical cancer be cured?
Yes, it can. Many women with stage 2 cervical cancer are cured, especially when treatment starts quickly. With proper treatment, there's a very real possibility of living a healthy, cancer-free life.
How serious is stage 2 cervical cancer?
It's understandable to feel worried. Stage 2 means the cancer has spread past the cervix, but it hasn't yet reached the pelvic wall. It's more serious than stage 1, but it's also still very treatable, and most women respond well to treatment.
Stage 1 often has minimal or no symptoms, while stage 2 typically causes more noticeable bleeding, discharge, or pelvic pain. Surgery is more common for stage 1, while radiation therapy with chemotherapy is usually the main treatment for stage 2.
What is the success rate of stage 2 cervical cancer treatment?
Treatment works well for about 60–75%. Your individual chances depend on things like tumour size, whether lymph nodes are involved, and how your body responds to treatment. Your doctor can give you a clearer picture based on your specific situation.
Can stage 2 cervical cancer spread?
Without treatment, stage 2 cervical cancer can continue to grow and spread to nearby areas in the pelvis, to lymph nodes, or even to other parts of the body. When this happens, it’s called metastatic cancer.
Cancer cells can travel through your lymphatic system, which is why starting treatment promptly is so important. Treatment stops the cancer from progressing and greatly reduces the chance of recurrent cervical cancer.
What are the long-term effects of stage 2 cervical cancer treatment?
Treatment can have lasting effects. You might experience early menopause if your ovaries are affected by radiation therapy, fertility loss with most treatments, and vaginal complications like dryness or discomfort. These effects are real, but they don't have to define your life after cancer. Your doctor can help you manage symptoms and maintain a good quality of life.
Will I be able to have children if I have cervical cancer?
Radiation therapy and radical surgery typically make pregnancy very difficult. However, if having children is important to you, there are options worth discussing before your cervical cancer treatment starts.
Egg or embryo freezing can preserve your ability to have biological children in the future. In some early-stage 2A1 cases, fertility-sparing surgery might be possible. It's best to talk to your doctor as soon as possible so they can find the right options for you.
What role does HPV play in cervical cancer?
HPV infection is the main cause of cervical cancer. HPV is a very common virus, and usually your body clears it on its own. Sometimes, though, the virus stays in the cervix and can cause changes to your cervical cells. These changes can lead to abnormal cells, and if they continue over many years, they may turn into invasive cervical cancer.
The HPV vaccine helps protect you from the types of HPV that cause most cervical cancers. Regular cervical cancer screening with a Pap smear can find abnormal cells early, before they develop into cancer.
The information is intended for general guidance only and should not be considered medical advice. For personalised recommendations and advice based on your unique situation, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
References:
Chen, X., Liang, W., Duan, H., Wu, M., Zhan, X., Dai, E., Lv, Q., Xie, Q., Liu, R., Xu, Y., Bin, X., Lang, J., Liu, P., & Chen, C. (2022). Discussion on the Treatment Strategy for Stage IIA1 Cervical Cancer (FIGO 2018). Frontiers in Oncology, 12, 800049. https://doi.org/10.3389/fonc.2022.800049
Chou, B., Venkatesulu, B. P., Coleman, R. L., Harkenrider, M., & Small, W., Jr. (2022). Management of stage I and II cervical cancer: a review. International Journal of Gynecological Cancer, 32(3), 216–224. https://doi.org/10.1136/ijgc-2021-002527
For more information, contact us:
Thomson Fertility Centre
- Paragon: 6252 7766
Thomson Specialists (Women's Health)
Thomson Women's Clinic
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
