Vaginal discharge is a normal part of your reproductive health. But changes in its colour, smell, or texture may be an indication of an underlying issue, such as sexually transmitted infections (STIs). If you've noticed these changes, it's natural to feel worried or uncertain.
However, the good news is that most cases of vaginal discharge caused by an STI can be treated. Let's take a closer look at this topic so you can make informed decisions and protect your sexual health.
What does normal vaginal discharge look like?
Vaginal discharge is a normal and healthy part of your reproductive system that helps keep the vagina clean, moist, and safe from infections. Normal vaginal discharge can look a little different for each person. Some people may see it as clear and slippery, like raw egg white, while others may see it as creamy, white, or pale yellow with a thicker texture.
The amount also varies, some people have a lot of discharge every day, while others have very little. A mild smell is usually normal, but discharge that doesn't smell at all is also healthy.
The discharge may change in appearance and texture during your menstrual cycle as oestrogen levels rise and fall. At the beginning or end of a period, it is common to see a pinkish or brown colour because of blood. Around the middle of the cycle or during ovulation, the discharge often becomes clear, stretchy, and slippery.
But sometimes changes in the colour, smell, or texture of discharge can mean that there is an infection, like an STI.
Which STIs cause abnormal vaginal discharge?
Several STIs can cause abnormal vaginal discharge, and each one has its own set of symptoms.
Chlamydia
Chlamydia is a common STI that is caused by the bacterium Chlamydia trachomatis. It can affect both men and women, and people often don't notice it because the symptoms are mild or absent.
Gonorrhoea
Gonorrhoea, caused by the bacterium Neisseria gonorrhoeae, can affect anyone who is sexually active, regardless of age or gender. Similar to chlamydia, many people don't know they have it because the symptoms can be mild or even go unnoticed.
Trichomoniasis
Trichomoniasis is a common, curable STI caused by the Trichomonas vaginalis parasite. The infection doesn't usually cause any symptoms in most people.
Mycoplasma genitalium
Mycoplasma genitalium is a bacterial infection that can look like chlamydia or gonorrhoea.
Bacterial vaginosis
Bacterial vaginosis is a common vaginal infection that happens when the bacteria in the vagina are not balanced. Bacterial vaginosis is not technically an STI, but it’s closely linked to sexual activity, and recent research suggests it may be sexually transmittable.
Herpes simplex virus (HSV)
Herpes simplex virus, or herpes, is a common infection that can cause painful sores or blisters. It can get into many parts of your body, but it most often affects your mouth and genitals.
Identifying STI vaginal discharge
The colour, consistency, smell, and other symptoms like itching, irritation, or pain of STI vaginal discharge can change depending on the type of infection.
Chlamydia
The discharge often looks like mucus, is a little yellow or cloudy, and doesn't smell very strong.
You might not know you have the infection until it is found during screening because symptoms are often not present.
Gonorrhoea
Causes discharge that is usually yellow or green and sometimes thick and like pus.
It often smells foul and can cause pain in the pelvis or when you pee.
Trichomoniasis
The discharge is usually frothy, yellow-green, and smells like fish.
Other symptoms may include itching, burning, redness, or pain around the vagina.
Bacterial vaginosis
The discharge is usually thin and greyish-white, and it smells strongly like fish, which is often more noticeable after intercourse.
Herpes
Vaginal discharge caused by herpes is usually mild, watery, or white.
Painful blisters or ulcers on or around the genitals, which may ooze fluid.
If you recognise any of these symptoms, schedule an appointment with Thomson Medical for a diagnosis and caring treatment in a safe, judgement-free environment.
What should you do if your vaginal discharge is not normal?

If you notice any unusual vaginal discharge, such as a change in colour, consistency, or smell, or if you have symptoms like itching, burning, pelvic pain, or pain during urination or sex, you should see a doctor right away. Unusual discharge may indicate the presence of STIs or another issue that requires diagnosis and treatment.
When you go to see a healthcare provider, the evaluation usually has a few steps.
Medical history and sexual health review
Your doctor will ask about your symptoms, sexual activity, birth control use, past sexually transmitted diseases (STDs), and any other health problems that might be important.
Pelvic examination
This allows your doctor to check for visible signs of infection, such as inflammation, lesions, unusual vaginal odour, or abnormal discharge.
Laboratory testing
Swab samples:
You can take them from the vagina or cervix to look for certain germs, like Chlamydia trachomatis or Neisseria gonorrhoeae.
Urine tests:
Urine tests can also aid in the detection of chlamydia or gonorrhoea.
Microscopy:
This is often used to look at discharge under a microscope, which can quickly find trichomoniasis or bacterial vaginosis.
Nucleic acid amplification tests (NAATs):
NAATs are special lab tests that look for the bacteria’s genetic material. They’re accurate and can spot an infection even when symptoms aren’t obvious.
NAATs are the best way to find chlamydia, gonorrhoea, and Mycoplasma genitalium.
Blood tests:
The tests are usually quick, painless, and give you important information so you can get the right treatment. Don’t be afraid to ask your doctor what tests they are doing and why you need them. Knowing how things work can make you feel more comfortable and in control.
It's not a good idea to diagnose and treat yourself because different infections can cause similar discharges but need very different medications. Getting an early and correct diagnosis not only makes sure that treatment works, but it also stops problems like pelvic inflammatory disease (PID), infertility, or passing the infection on to your partner.
Our sexual health specialist
Loading...
How to deal with STI vaginal discharge
The treatment you need depends on the type of infection causing the discharge. Here are some common examples:
Chlamydia:
Usually treated with antibiotics like azithromycin or doxycycline.
Gonorrhoea:
Needs stronger antibiotics, often a combination of an injection and oral medicines.
Trichomoniasis:
Treated with a special medicine called metronidazole that kills parasites.
Herpes:
As of now, there is no definitive cure yet, but antiviral drugs like aciclovir can help keep outbreaks under control and make symptoms less severe.
Bacterial vaginosis:
Treated with antibiotics like metronidazole or clindamycin.
Don’t try to treat yourself or buy medicine on your own, since different infections can cause the same symptoms, and taking the inappropriate medicine can make the conditions worsen. Always talk to a healthcare professional about the right diagnosis and treatment.
Schedule an appointment with our O&G specialists at Thomson Medicalto discuss your symptoms and receive the right tests for early detection and effective treatment.
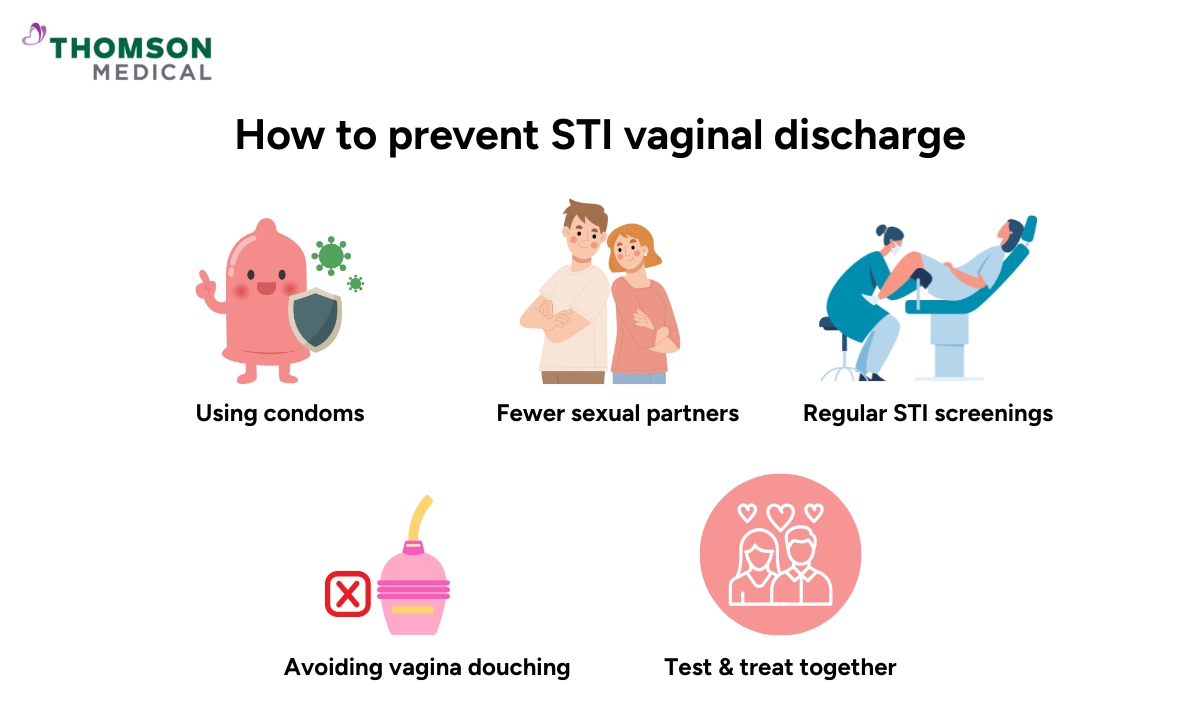
Preventing STI vaginal discharge
Taking care of your vaginal health and practicing safer sex can keep STI vaginal discharges from happening. There is no one way that works 100% of the time, but the following tips can help you.
Use condoms during sexual intercourse
Condoms stop the exchange of blood, vaginal fluids, and semen during intercourse. This barrier stops STIs from spreading by keeping viruses and bacteria out. Using condoms from start to finish during vaginal, anal, and oral intercourse is the best way to stay safe.
Limit the number of sexual partners
The more partners you have, the more likely you are to get STIs. You can lower your risk by having fewer partners and making sure you know their sexual health status.
Get regular STI screenings
Chlamydia and gonorrhoea are two STIs that can cause vaginal discharge, but they don't always show symptoms. It's important to get regular STI screening, especially if you have a new or more than one sexual partner. Early detection speeds up treatment, stops symptoms from happening, and lowers the risk of passing STIs to your partner.
Don't wash your vagina
Some women wash or rinse (douche) their vagina because they think it helps keep it clean, but in reality, douching throws off the natural balance of bacteria in the vagina. This makes it easier for harmful bacteria and viruses to grow, which raises the risk of infections and unusual discharge. Instead, you should wash the outside of your genitals gently.
Encourage your partner to get tested and treated
You could still get an STI again if your partner has one that hasn't been treated, even if you get tested and treated. Talking openly with your partner about sexual health, testing, and treatment is an important step to keep both of you safe.
FAQ
Are symptoms always present if I have an STI?
No. Many STIs, like chlamydia and gonorrhoea, don’t show any symptoms in the early stages. This means you could have the infection and not even know it. It is important to have regular screening, especially if you have new or multiple sexual partners, to find and treat STIs early.
What vaginal discharge is normal?
Normal vaginal discharge plays an important role in keeping the vagina clean and healthy. It is usually:
- Clear, milky-white, or slightly cloudy
- Mild or no odour
- Changes a little during your menstrual cycle (for example, thinner and stretchy around ovulation, thicker before or after a period)
If your discharge becomes yellow, green, grey, frothy, smells bad, or hurts or itches, it could be an STI or another infection.
Why is it important to treat abnormal discharge caused by an STI?
If you don't get treatment for STIs, they can have serious long-term effects. Chlamydia and gonorrhoea are two infections that can spread to the uterus, fallopian tubes, and ovaries. Such infections can cause pelvic inflammatory disease (PID), which can result in constant pelvic pain, infertility, or ectopic pregnancy.
Also, STIs can make it easier to get or spread HIV. Infections can be passed on to sexual partners or, if a woman is pregnant, to her baby during childbirth. Taking care of the infection keeps you and others healthy.
Will vaginal discharge from an STI go away without treatment?
No, most of the time. Some symptoms might get better on their own for a while, but the infection usually stays in your body and can come back or get worse over time. For instance, chlamydia or gonorrhoea that isn't treated can harm the reproductive system without causing any symptoms or making them go away. So, you almost always need medical care.
How is STI screening for abnormal discharge done?
When you visit a healthcare provider with an unusual discharge, they’ll usually do a few simple checks and tests to find out what’s wrong. These tests are quick, safe, and give clear answers so you can get the right care.
- Swabs:
- A small swab can be used to take a sample from the vagina or cervix to look for signs of bacterial, viral, or parasitic infections.
- Urine tests:
- To find infections like chlamydia and gonorrhoea without having to take samples from the body.
- Microscope checks:
- To find infections like trichomoniasis or bacterial vaginosis.
- Advanced lab tests (nucleic acid amplification tests - NAATs):
- These tests are very accurate and can find even small amounts of bacteria that cause STIs.
- Blood tests:
- If your doctor thinks you might have HIV, syphilis, or herpes, they may also suggest a blood test.
What colour is an STI discharge?
The colour, smell, and texture of discharge can give clues about the underlying infection:
- Yellow or green:
- Often linked to gonorrhoea or trichomoniasis, sometimes thick and pus-like.
- Grey-white:
- Common in bacterial vaginosis, usually with a fishy smell.
- Cloudy or whitish:
- Could be a sign of chlamydia or herpes, which are sometimes mild and go unnoticed.
- Clear:
- Can be normal, but if it comes with pain, burning, or sores, it may still suggest an infection.
It's good to know these differences, but discharge alone can't tell you which STI you have. So, it’s important to be examined and tested by a healthcare professional.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and advice based on your unique situation, please consult a specialist at Thomson Medical.Schedule an appointment with Thomson Medical today.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
