Have you ever experienced itching or unusual discharge after being intimate with your partner? If so, you may have a yeast infection, which is a common condition that affects many sexually active women.
While yeast infections aren't sexually transmitted, sexual intercourse can sometimes trigger them by disrupting your vaginal balance, making it easier for yeast to overgrow. Understanding the connection between sexual activity and these infections can help you prevent and manage these uncomfortable episodes more effectively.
Can sexual intercourse cause a yeast infection?
Yes, intercourse can sometimes trigger or cause a yeast infection, but this is not always the case. Yeast infections are typically caused by an overgrowth of the fungus Candida albicans, which naturally exists in the body, especially in the vagina. Certain factors can make the vaginal environment favourable for this overgrowth, and intercourse can sometimes contribute to it.
Why do some people develop yeast infections after sex?
Several factors related to sexual activity can disrupt the delicate balance in the vaginal environment, making it easier for yeast to overgrow. Here are the main reasons:
Change in vaginal pH:
Semen can alter the vaginal pH, making it more alkaline, which can encourage the overgrowth of yeast. The normal vaginal environment is typically acidic, which helps keep yeast levels in check.
Friction and irritation:
The physical movement during intercourse can cause friction that may irritate the vaginal lining. This irritation can disrupt the balance of bacteria and yeast in the vagina, increasing the likelihood of a yeast infection.
Moisture:
If the vagina becomes overly moist or sweaty during intercourse and isn’t properly dried afterward, this creates a warm, damp environment where yeast can thrive.
Antibiotics:
Taking antibiotics, whether to treat your infection or as part of your partner’s treatment plan, can upset the vaginal bacteria balance, making yeast infections more likely.
Diabetes:
High blood sugar levels from uncontrolled diabetes can lead to an increased risk of yeast infections. This can be especially noticeable after sexual activity.
New sexual partners or different intimate products:
Using new lubricants, spermicides, or having a new sexual partner can introduce different bacteria or chemicals that disrupt your normal vaginal flora.
Symptoms of a yeast infection
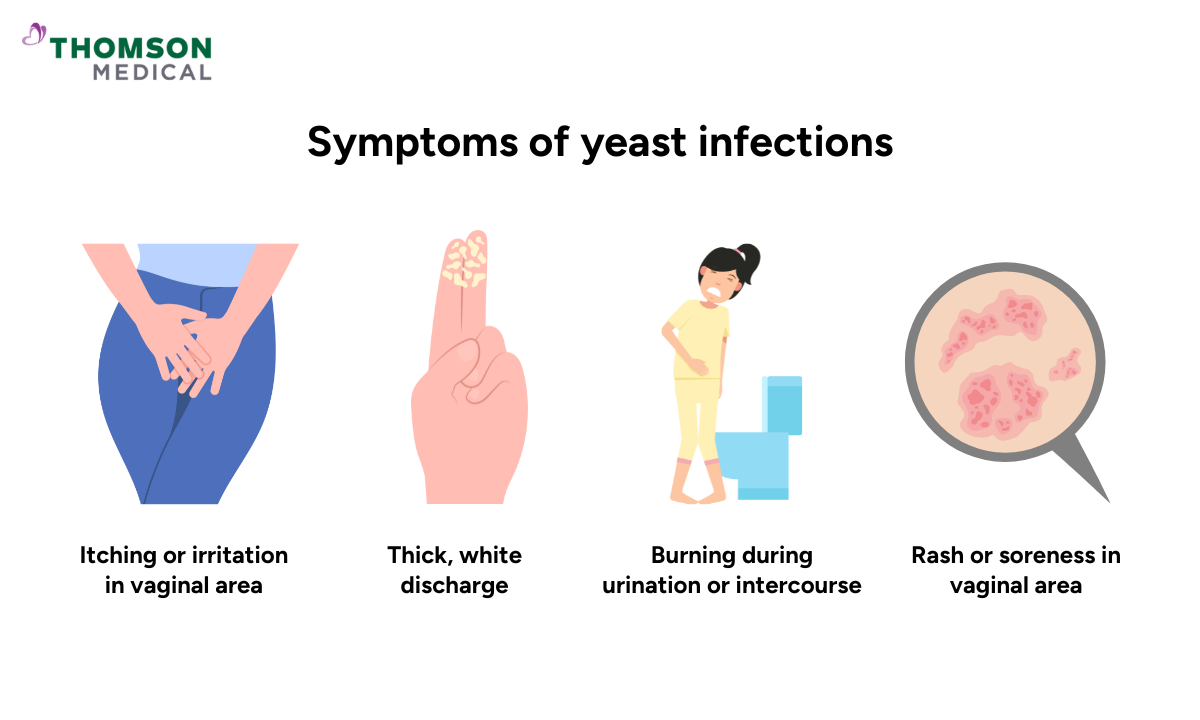
Although yeast infections are common, recognising their symptoms early can help you seek treatment promptly. The symptoms of a yeast infection include:
Itching or irritation in the vaginal area
Thick, white discharge that resembles cottage cheese (often odourless)
Burning during urination or intercourse
Redness or swelling of the vulva (the outer part of the vagina)
Pain or discomfort during intercourse
Rash or soreness around the vaginal area
If you're experiencing recurring yeast infections, severe symptoms, or symptoms that aren't improving with treatment, don't hesitate to consult a specialist. At Thomson Women’s Clinic, our specialists can help identify the underlying cause and provide treatment tailored to your needs. Schedule an appointment today.
Difference between yeast infections and STIs
While a yeast infection and a sexually transmitted infection (STI) may share some symptoms, understanding the difference is important for proper treatment. Here's how they differ:
Yeast Infection:
Caused by an overgrowth of naturally occurring yeast (Candida), which is usually triggered by antibiotics, changes in hormones, or a weakened immune system. It's not an STI.
STIs:
STIs are caused by bacteria, viruses, or parasites that are transmitted from one person to another through sexual contact.
Symptoms of STIs can include abnormal discharge, pain during sex or urination, sores, rashes, and more, depending on the infection.
Our sexual health specialists
Loading...
When to see a doctor for a yeast infection
Yeast infections are usually manageable at home, but certain situations require professional medical attention. You should see a healthcare provider if you are experiencing:
First-time symptoms:
It could be your first yeast infection, and you're unsure what's going on.
Persistent symptoms:
If symptoms don't improve after using over-the-counter treatments.
Frequent infections:
If you experience frequent or recurring yeast infections (more than 4 times a year).
Severe symptoms:
If you have severe pain, swelling, or redness that doesn't go away.
Unusual symptoms:
If you have an unusual discharge with a foul odour or pain that doesn't feel like typical yeast infection discomfort, you might be dealing with STIs or other medical conditions.
Treatment for yeast infection after sex

The good news is that yeast infections are treatable with several effective options. Treatment options include:
Over-the-counter antifungal medications:
These can be purchased as creams, ointments, or suppositories. Common ones include miconazole nitrate or clotrimazole.
Prescription antifungal pills:
Your doctor may prescribe oral medications like fluconazole if your yeast infection is severe or recurrent.
How to prevent yeast infections after sex
Taking preventive steps can significantly reduce your risk of developing a yeast infection after sexual activity. Here's what you can do:
Use condoms:
Condoms can help reduce the risk of introducing new bacteria or altering the vaginal environment.
Maintain good hygiene:
Gently wash your vulva area with unscented soap and warm water after intercourse. Avoid douching or washing inside your vagina.
Avoid scented products:
Scented soaps, sprays, and hygiene products can irritate the delicate vaginal tissues, making yeast infections more likely.
Wear breathable cotton underwear:
Avoid tight, synthetic fabrics that trap moisture and heat in the genital area.
Keep the area dry:
After sexual intercourse or exercise, change out of any wet or sweaty clothes to prevent moisture buildup that can lead to yeast infections.
Stay hydrated:
Drinking plenty of water helps maintain a healthy balance of bacteria and yeast in the body.
For further guidance on managing yeast infections, schedule an appointment with Thomson Women’s Clinic. Our specialists will work with you to find the most suitable treatment approach for your condition.
FAQ
Can I have intercourse while treating a yeast infection?
It's generally best to avoid sexual intercourse during a yeast infection, especially if it's painful or if you're using antifungal medications. It can also prevent irritation and help reduce the spread of the infection to your partner.
Can I pass a yeast infection to my partner?
While yeast infections are not sexually transmitted, it's possible to pass them back and forth if one of you has them. Even though yeast infections are common and not considered STIs, sexual contact can spread the yeast, particularly if you're engaging in unprotected intercourse.
Can a man cause a woman a yeast infection?
While men don't typically get yeast infections, they can carry the yeast on their genitals (without symptoms) and pass it to a partner during sexual intercourse. It's always a good idea for both partners to be treated if one of you has a yeast infection to avoid reinfection.
Do condoms prevent yeast infections?
Condoms can reduce the risk of a yeast infection by limiting the introduction of outside bacteria and by preventing semen from changing the pH of the vagina. They don't completely eliminate the risk but do reduce the chances.
Why do I always get yeast infections after sex?
Frequent yeast infections after sex can result from various factors. These include:
- Frequent antibiotic use
- Uncontrolled diabetes
- Hormonal fluctuations (e.g., birth control or pregnancy)
- Sensitivity to certain products like lubricants or condoms
- Stress or weakened immune system
Consider seeing a doctor for more tailored advice.
Can a diet consisting of sugar and alcohol increase the risk of yeast infections?
Yes, diet can play a role in yeast infections. High sugar intake can encourage the growth of yeast, as yeast feeds on sugar, while alcohol can disrupt the immune system and promote yeast overgrowth. A balanced diet with minimal sugar and alcohol can help reduce the risk of yeast infections.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice based on your unique situations, consult a specialist at Thomson Women’s Clinic. Schedule an appointment today.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
