Have you ever been worried about whether unusual vaginal bleeding or discharge could mean cervical cancer or uterine cancer? You're not the only one who is worried about this. In fact, this kind of worry isn’t a negative thing. It shows that you care about your health and are paying attention to your body.
Cervical cancer and uterine cancer are two of the most common gynaecological cancers. Although they both occur in the uterus area, they have different causes, risk factors, symptoms, and treatment options. Knowing these differences can help you notice early warning signs, seek timely care, and protect your long-term health.
What is cervical cancer?
Cervical cancer begins in the cervix, which is the lower, narrow part of your womb that connects to your vagina.
The main cause of cervical cancer is a persistent infection with high-risk types of human papillomavirus (HPV), a very common virus spread through sexual contact. In most cases, HPV infections clear on their own. But when the virus stays in your body, it may cause abnormal cell changes in your cervix, which can slowly develop into cancer if left untreated.
What is uterine cancer?
Uterine cancer, also known as endometrial cancer, starts in the lining of your womb.
Unlike cervical cancer, this cancer is not linked to HPV. Instead, it is usually related to hormonal imbalance, especially when there is too much oestrogen without enough progesterone to balance it out. This imbalance can lead to thickening of the uterine lining and eventually allow cancer cells to develop.
Cervical cancer vs uterine cancer: key differences
Feature | Cervical cancer | Uterine (endometrial) cancer |
Location | Cervix (lower part of your womb) | Lining of your womb |
Main cause | Persistent high-risk HPV infection | Hormonal imbalance (excess estrogen) |
Typical age group | 30–50 years (reproductive age) | 50+ years (postmenopausal age) |
Primary risk factors | HPV, smoking, multiple partners, early sexual activity | Obesity, diabetes, unopposed estrogen, late menopause |
Link to HPV | Strongly associated | Not associated |
Prevention | HPV vaccination, Pap smear screening | Weight management, hormone balance, early evaluation of abnormal bleeding |
Early detection method | Pelvic ultrasound, endometrial biopsy | |
Main symptom | Bleeding after sex, irregular bleeding, pelvic pain | Postmenopausal bleeding, heavy or prolonged periods |
Treatment | Surgery, radiation therapy, chemotherapy | Surgery, hormone therapy, radiation therapy |
Cervical cancer vs uterine cancer: Which is more common?
Cervical and uterine cancers are both important women’s health concerns, but their patterns differ across the world. Uterine cancer is more common in many developed countries. This is partly because women often go to the doctor right away when they have postmenopausal bleeding, which makes it easier to find.
In contrast, cervical cancer tends to be more common in many developing countries, where limited access to HPV vaccination and regular screening can delay diagnosis.
What’s it about in Singapore? Let’s look more closely at how common each cancer is among women in Singapore.
Cervical cancer | Uterine cancer | |
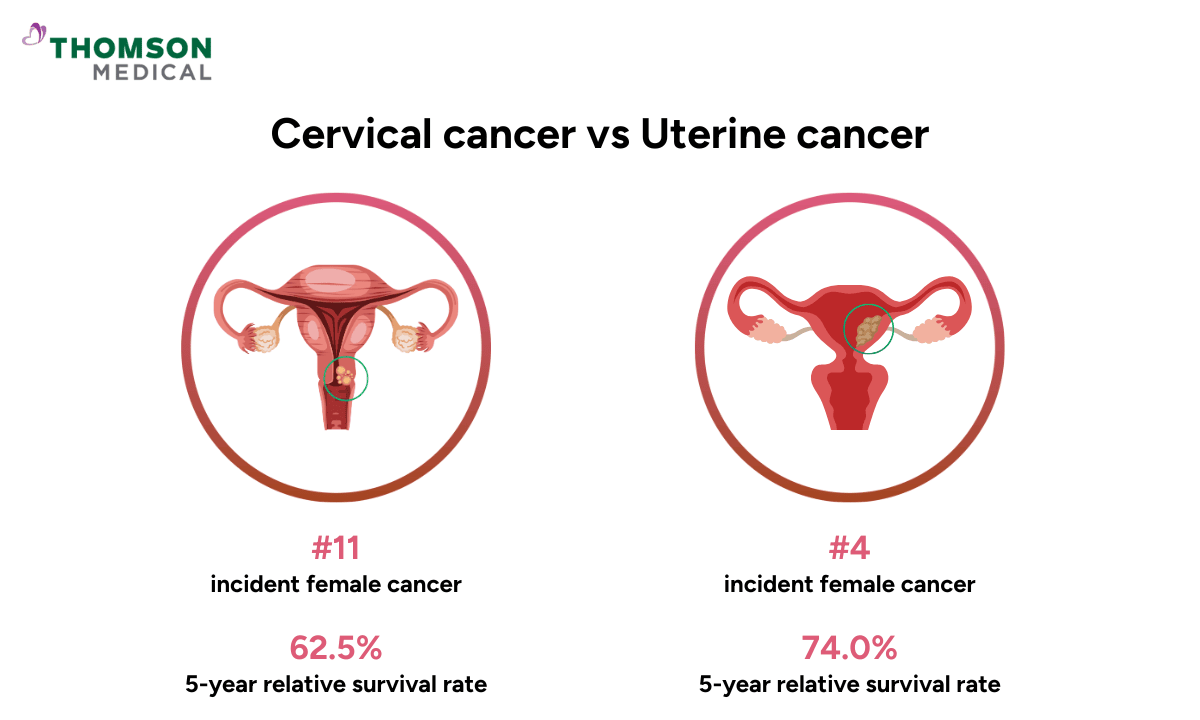
Ranking among Singaporean women | 11 | 4 |
% of all female cancers | 2.5 | 7.4 |
New cases per year | 1,120 | 3,310 |
The table shows that uterine cancer is much more common than cervical cancer in Singapore. There are almost three times as many new cases each year. This shows the importance of paying close attention to unusual symptoms, especially for women in their 50s to 70s, who are most likely to be affected.
On the other hand, cervical cancer occurs less frequently, partly thanks to HPV vaccination and regular cervical cancer screening. However, it still affects many women, especially younger ones. That's why regular Pap tests, HPV tests, and HPV vaccinations are important for early detection and prevention.
Regular screening saves lives. If you’re due for your Pap smear or HPV test or just want peace of mind, schedule a women’s health screening at Thomson Medical. Our specialists provide gentle, personalised care to help you stay healthy at every stage of your life.
Our women's cancer specialist
Loading...
Cervical cancer vs uterine cancer: Which has a higher survival rate?
Both cancers are highly treatable when detected early, but their outlooks differ slightly. Uterine cancer generally has a higher survival rate because its early warning signs often prompt women to seek medical care sooner. Cervical cancer, on the other hand, can progress quietly for years without noticeable symptoms.
In Singapore, the five-year relative survival rate is about 62.5% for cervical cancer and approximately 74.0% for uterine cancer.
Warning signs of cervical and uterine cancer
You might be wondering if, since both cervical cancer and uterine cancer occur in the same area of the female reproductive system, there are any signs that help tell them apart. The answer is yes. While some symptoms can seem similar, each cancer still has slightly different warning signs.
What does cervical cancer look like?
High-risk HPV can take decades to cause cervical cancer. That is why cervical cancer often grows slowly and may not show any signs at an early stage. When symptoms do appear, they could include changes like:
Abnormal vaginal bleeding:
You may notice spotting between periods, bleeding after sexual intercourse, or any bleeding after menopause.
Unusual vaginal discharge:
Your vaginal discharge becomes wet, bloody, or has a strong odour.
Ongoing pain:
Persistent pelvic or back pain, discomfort during sex, or a feeling of pressure in the lower abdomen may also occur.
Urinary issues:
You may experience frequent or urgent urination, pain, or difficulty passing urine.
Leg swelling:
One or both legs are swelling if the cancer presses on nearby nerves or blood vessels.
What does uterine cancer look like?
Uterine cancer often shows warning signs earlier than cervical cancer. Here are some symptoms that you may experience:
Vaginal bleeding after menopause:
This is one of the most common and earliest symptoms of uterine cancer, even if it’s just light spotting.
Abnormal vaginal bleeding:
If you are still menstruating, you may notice heavy or unusually prolonged periods, or bleeding between menstrual cycles.
Pelvic pain:
Some women experience pelvic pain or a sensation of pressure, which may become more noticeable over time.
Unusual vaginal discharge:
You may have watery or bloody discharge.
Persistent tiredness or unexplained weight loss:
These symptoms usually appear in more advanced stages.
When should you see a doctor

Your body often gives you small clues when something isn’t right. While not every symptom means cancer, it’s important not to ignore persistent changes. You should see a doctor if you notice the following symptoms:
Vaginal bleeding after menopause
Bleeding between menstrual cycles or after sex
Persistent pelvic pain or pressure
Unusual vaginal discharge
Painful intercourse
If you’ve noticed any unusual bleeding, pelvic discomfort, or changes in your body that don’t feel normal, don’t wait or worry alone. Schedule an appointment with our gynaecologists at Thomson Medical. We're here to listen and provide personalised evaluations so you can get the timely care you need.
FAQ
Can you have cervical cancer and uterine cancer at the same time?
Yes, it is rare, but it can happen. Cervical cancer and uterine cancer start in different tissues, so a woman can develop both conditions independently. When this situation occurs, each cancer needs to be evaluated and treated separately based on its type and stage.
Are endometrial cancer and uterine cancer the same?
Yes, endometrial cancer is the most common form of uterine cancer. It begins in the lining of the uterus, so the terms “endometrial cancer” and “uterine cancer” are often used interchangeably.
What does the endometrium do?
The endometrium is the inner layer of your womb. Each month, it thickens in preparation for supporting embryo implantation and nourishing an early pregnancy. If pregnancy does not occur, this lining breaks down and is shed during menstruation.
Can you live 10 years after cervical cancer?
Yes, many women live well beyond 10 years after cervical cancer treatment, especially if diagnosed early. Early-stage cervical cancer has a high cure rate, as it often responds very well to surgery or chemoradiation.
How fast does cervical cancer spread?
Cervical cancer usually develops slowly. Precancerous changes can take 10–20 years to progress to cancer. However, once the disease becomes invasive, it can spread more quickly to nearby tissues or, in advanced cases, to distant organs. This is why regular cervical cancerscreening is important.
Can you be completely cured of cervical cancer?
Yes, if detected early, cervical cancer is highly curable through surgery, radiation therapy or chemoradiation. Even some later-stage cases can be successfully treated with modern therapies.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and advice based on your unique situation, please consult a specialist at Thomson Medical.Request an appointment with Thomson Medical today.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) - Jurong:
6262 8588 (Call), 6262 8588 (WA) - Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
Notice
The range of services may vary between TWC/TS locations. Please contact your preferred branch directly to enquire about the current availability.
Request an Appointment