One of the biggest worries that many HIV-positive women share is the fear of developing other infections or illnesses, especially HPV and cervical cancer.
If this has been on your mind, please know that you’re not alone. Many women share the same concerns – and it’s perfectly understandable to feel unsettled.
But living with HIV does not mean that cervical cancer is something you will inevitably face. With regular screening, consistent HIV treatment and timely follow-up, many women continue to live long, healthy and full lives.
How HIV increases cervical cancer risk
Cervical cancer usually develops after a long-lasting infection with high-risk types of human papillomavirus (HPV), most commonly HPV 16 and 18. In most women, the immune system clears HPV naturally within one to two years.
However, HIV affects your immune system in ways that make HPV infection more persistent, and your cervical cancer risk is up to six times higher than HIV-negative women.
Here’s why HIV may increase your chances of developing cervical cancer:
HIV weakens your immune system:
HIV lowers your CD4 cell count (a measure of immune strength) and makes it harder for your body to clear HPV naturally.
Persistent high-risk HPV infections:
High-risk HPV infections may last for many years due to your weakened immune system, giving abnormal cervical cells more chance to develop into cancer.
Multiple HPV types:
Women living with HIV are more likely to carry multiple HPV types, including the high-risk strains.
High risk of recurrence:
Even after treatment for precancerous lesions, recurrence is more common in HIV-positive women.
Even though the risk is higher, staying consistent with ART and routine screening puts you in a much stronger and safer position.
Cervical cancer screening for women living with HIV
Living with HIV can sometimes make you feel like your body is more vulnerable, but cervical cancer screening is one powerful way to take back control. These tests can pick up precancerous changes on your cervix long before they turn into cancer – at a stage when treatment is simple, gentle, and highly effective.
By going for regular screening, you’re giving yourself the best chance to stay healthy, be there for your loved ones, and plan your future with more peace of mind.
Here are screening recommendations for HIV-positive women that your doctor may recommend:
Start screening as soon as you are diagnosed with HIV, regardless of your age
Pap smear every 6–12 months in the first year after HIV diagnosis.
Annual Pap smears if the first two tests are normal
HPV testing for women aged 30 and above
Colposcopy and biopsy if any abnormal results appear
Cervical cancer symptoms in HIV-positive women
Symptoms of cervical cancer can look the same whether you live with HIV or not, but they may appear earlier. If you notice any of the following, try not to panic – most causes are treatable, but it’s important to get checked.
Abnormal vaginal bleeding (after intercourse, between periods, or after menopause)
Watery or foul-smelling vaginal discharge
Pelvic pain or discomfort during intercourse
Back or leg pain, leg swelling, or fatigue in more advanced stages
If you notice any of these symptoms – even if your most recent Pap smear was normal – consult your doctor promptly. Early evaluation can make a tremendous difference.
If you’re living with HIV and have noticed any unusual symptoms, schedule an appointment at Thomson Medical for a thorough, personalised evaluation. Our gynaecology specialists will help you feel safe, supported, and fully informed at every step.
Our cervical cancer specialist
Loading...
Treatment options for cervical cancer in HIV women
The good news is that treatment for cervical cancer in women living with HIV is similar to treatment for women without HIV. The main difference is that your doctor will take additional steps to make sure your treatment plan is safe for your immune system and works alongside your HIV medication.
Surgery
For early-stage cervical cancer (stage 0 or stage 1A), your doctor may recommend LEEP, conisation or hysterectomy. When your CD4 count is stable and your viral load is under control, these treatments are usually safe.
Radiation and chemotherapy
For more advanced stages, you may need a combination of radiation therapy and chemotherapy. Your doctor will carefully monitor drug interactions between chemotherapy and HIV medications to keep you safe throughout treatment.
Antiretroviral therapy (ART)
Staying on ART throughout your cancer treatment is essential – it helps your body stay strong and respond better to therapy. A strong immune system helps your body respond better to cancer treatment, reduces the chance of HPV-related changes progressing, and lowers the risk of recurrence.
Keep in mind that women who remain stable on ART often experience excellent treatment outlooks.
How to prevent cervical cancer with HIV
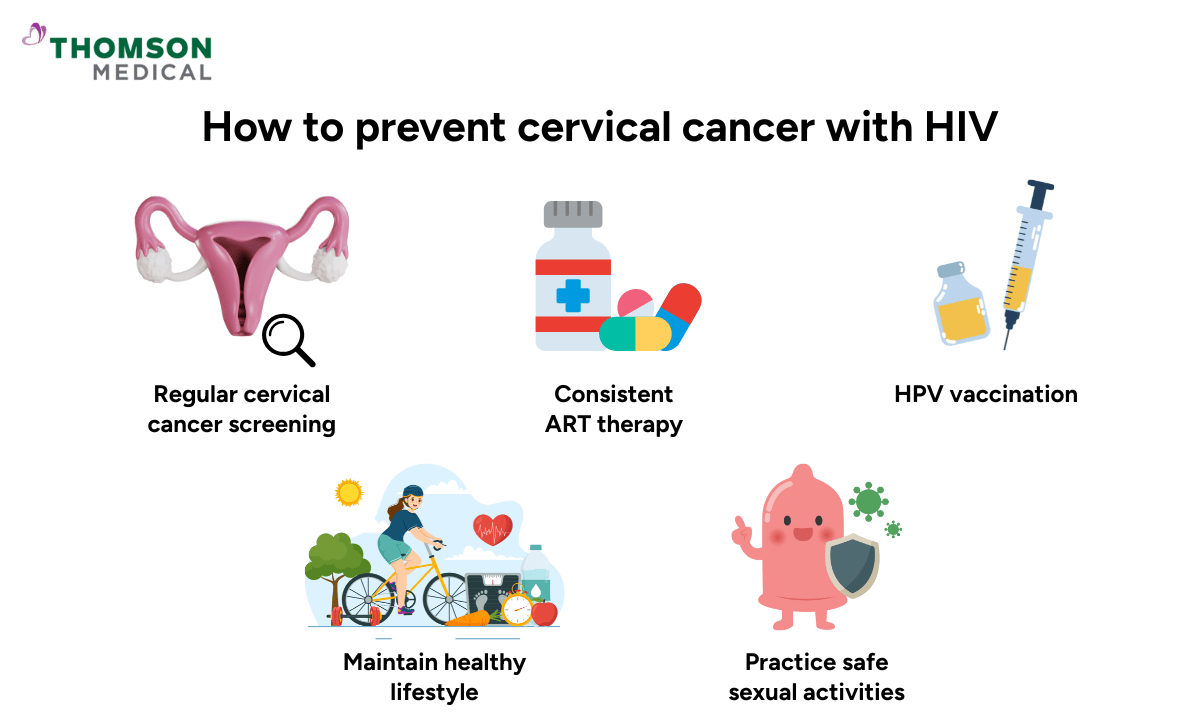
Living with HIV and managing cervical cancer risk may feel daunting at times, but it does not have to define your life. You can significantly lower your risk with proper preventive care. Many women with HIV lead healthy, cancer-free lives for decades.
Regular cervical cancer screening
Early detection of cervical cancer leads to highly effective treatment, making it one of the most crucial steps you can take. Do not skip screening even if you feel well.
Consistent ART therapy
Keeping your viral load low and your CD4 count high is an effective tool for preventing cervical cancer. ART reduces HPV persistence and slows the progression of abnormal cervical cells.
HPV vaccination
The HPV vaccine protects against high-risk HPV types such as HPV 16 and 18. It is recommended for women living with HIV under medical supervision. Even if you already have HIV or have had HPV, vaccination can still provide protection against other strains.
Maintain healthy lifestyle
A strong immune system helps your body fight infections and recover more effectively. You can maintain a healthy lifestyle to boost your immunity by:
Eating a balanced, antioxidant-rich diet
Avoiding smoking and limit alcohol
Exercising regularly
Getting adequate rest and managing stress
Practice safe sexual activities
HPV is a common virus passed through sexual contact. Using condoms helps you reduce the risk of HPV reinfection and protects against other sexually transmitted infections (STIs), which can further weaken your immune system.
Looking after your general health can make a meaningful difference. Eating well, staying active and avoiding smoking all help keep your immune system strong.
If you're living with HIV and want personalised, compassionate support for cervical cancer screening and prevention, our gynaecologists at Thompson Medical are here to help. Book an appointment today to receive attentive care and guidance tailored to your individual health needs.
FAQ
What is the relationship between HIV and cervical cancer?
HIV and cervical cancer are closely linked because HIV weakens your immune system, making it much harder for your body to clear human papillomavirus (HPV) infections. Over time, this increases the chance of abnormal cells developing and progressing to cervical cancer.
Can cervical cancer be prevented in HIV-positive women?
Yes, even if you are living with HIV, cervical cancer is often preventable – or treatable at an early stage – when you follow a regular Pap smear or HPV testing, ART adherence, HPV vaccination and a healthy lifestyle.
How often should HIV-positive women be screened?
Screening is even more important if you have HIV, as changes in the cervix can develop more quickly. The general recommendations are:
At HIV diagnosis: Have your first Pap smear
During the first year: Repeat screening every 6–12 months
After two normal results: Continue with annual Pap smears
If your doctor finds any abnormalities, they may suggest more frequent testing or a colposcopy for a more thorough evaluation.
Does successful HIV treatment reduce cervical cancer risk?
Yes, ART helps increase your CD4 count, keep your viral load low, and strengthen your body’s ability to fight off HPV infections. Women with well-controlled HIV have a much lower chance of developing severe cervical changes or cancer compared to those with untreated or poorly controlled HIV.
Can the HPV vaccine help if you already have HIV?
Even if you already have HIV, the HPV vaccine can still provide valuable protection by preventing infections from HPV types you have not yet encountered. It can also reduce the risk of reinfection and future HPV-related disease.
What are the most common cancers in HIV women?
Women living with HIV are more likely to develop certain cancers, especially those linked to viral infections. The most common include:
Cervical cancer
Kaposi’s sarcoma
Non-Hodgkin lymphoma
Anal cancer
What role does CD4 count play in cervical cancer development?
Your CD4 count reflects the strength of your immune system. When CD4 levels are low – especially below 200 cells/mm³ – your body struggles to clear HPV infections, making it more likely for abnormal cervical cells to develop and progress. Keeping your CD4 count healthy through regular ART is one of the best ways to protect your cervical health.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and advice based on your unique situation, please consult a specialist at Thomson Medical.Request an appointment with Thomson Medical today.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
