Cervical cancer can remain hidden for many years – a fact that naturally worries many women. Without any clear signs or symptoms to watch out for, it's normal to feel concerned about what might be happening in your body.
The good news is that cervical cancer usually develops slowly. This gradual process means there is often time to detect abnormal cell changes early through regular screening. Understanding how long cervical cancer takes to grow can help ease anxiety and support you in taking the right steps at the right time for your health.
How long does cervical cancer take to develop?
Cervical cancer typically develops gradually, usually over a span of 10 to 15 years – giving you plenty of time to detect and address changes early.
It begins with a human papillomavirus (HPV) infection, which may cause cells in the cervix to change over time.
Regular cervical screening remains one of the most effective ways to monitor your cervical health and detect any changes early, when they're most treatable.
Connection between HPV and cervical health
There are over 100 types of HPV, but only about 14 are considered high-risk for cervical changes. Your body is actually very good at clearing HPV on its own, and most infections go away naturally within one to two years without causing any problems.
Sometimes a high-risk type can linger in the body instead of clearing. When this happens, it may slowly cause changes to your cervical cells. If these changes aren't picked up through cancer screening, they could eventually develop into cervical cancer.
Stages from HPV to cervical cancer
Cervical changes happen gradually in stages, and understanding them can help you feel more in control of your cervical health:
Initial HPV infection:
Most sexually active people will get HPV at some point in their lives.
Your immune system usually clears the virus on its own without you even knowing you had it.
In some cases, a high-risk HPV type like 16 or 18 can persist in the body, increasing the chance of cervical changes developing over time.
Precancerous changes:
If HPV remains there, it can cause abnormal changes in your cervical cells called cervical intraepithelial neoplasia (CIN):
CIN 1: Mild changes that often go away by themselves without any treatment.
CIN 2: Moderate changes. Your doctor may recommend monitoring or treatment depending on your situation.
CIN 3: More significant changes that need treatment to prevent them from potentially developing into cancer.
These changes typically develop slowly over several years, giving you time to detect them through regular screening.
Invasive cancer:
If precancerous changes aren't detected and treated, they can progress into invasive cervical cancer, where cancerous cells spread beyond the surface of the cervix.
This progression usually takes a decade or longer, though it can occasionally happen faster.
Keeping up with your screening appointments is one of the most caring things you can do for yourself, as it helps catch changes early, when they're most manageable.
Not sure if you have HPV or cervical cell changes? Request an appointment with Thomson Medical and we will guide you through the right screening options for your age and risk factors.
How fast can it progress?
Progression can be faster when the virus persists and the cervix is exposed to factors that make it harder for the body to control abnormal cell changes.
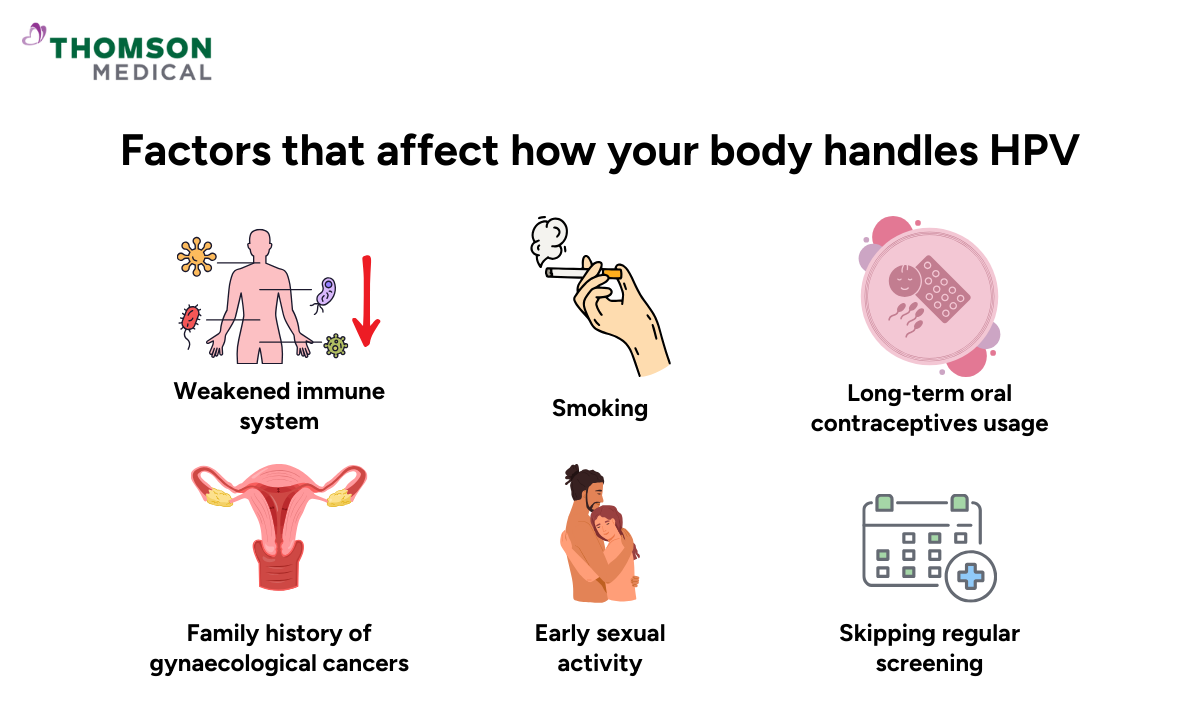
Factors that may affect how your body handles HPV:
A weakened immune system from conditions like HIV, immunosuppressing medicines, or poor nutrition
Smoking, which affects your cervix's ability to heal and clear HPV
A persistent high-risk HPV infection that hasn't cleared
Skipping regular screenings, meaning that changes go unnoticed for longer
Other infections like chlamydia that cause cervical inflammation
Long-term oral contraceptive use or having had multiple full-term pregnancies
Early sexual activity or multiple partners, increasing HPV exposure
A family history of cervical or gynaecological cancers
If any of these apply to you, it's important to remember that this does not mean you are guaranteed to develop cervical cancer. They're simply a reminder of why screening is so valuable for you – catching any changes at their earliest, most treatable stage.
Early warning signs of cervical cancer
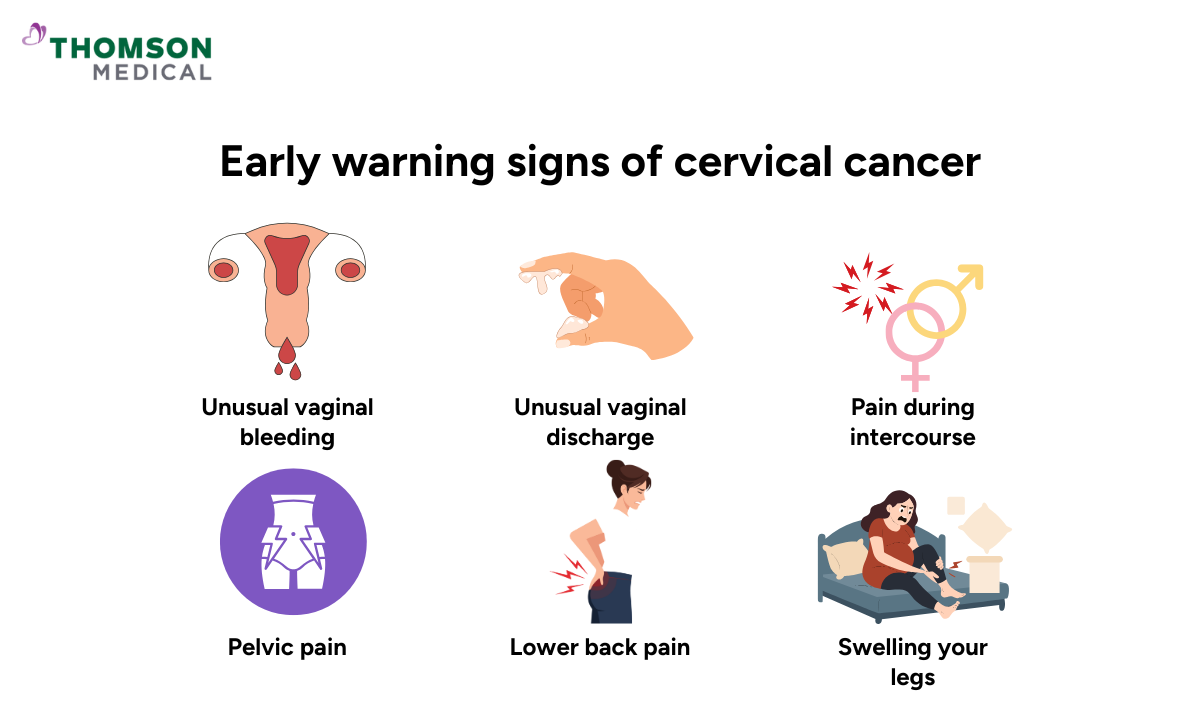
Cervical cancer rarely causes symptoms in its early stages, which is exactly why regular screening matters so much. As changes progress, you might notice:
Unusual vaginal bleeding, like bleeding after intercourse, between periods, or after menopause
Vaginal discharge that's different from usual, perhaps watery, blood-tinged, or with an unusual smell
Discomfort or pain during intercourse
Persistent pelvic or lower back pain
Swelling or pain in your legs, though this typically happens in more advanced stages
These symptoms don't automatically mean cancer. They're often caused by other, much less serious conditions, which can make it harder to identify the true cause.
Notice something that doesn't feel quite right? Don't hesitate to get it checked. Whether it turns out to be a minor concern or nothing at all, you deserve the reassurance that comes with knowing for certain.
Our cervical cancer specialist
Loading...
How screening protects you
Regular cervical screening is one of the most effective ways to prevent cervical cancer. It catches precancerous changes early, often years before they could develop into anything serious.
The two main screening tests are:
Pap test (Pap smear) checks for abnormal cervical cells
HPV test checks for high-risk HPV types that could affect your cervical health
Recommended screening schedule in Singapore:
If you've ever had sexual intercourse, here's what's recommended:
Ages 25 to 29: Pap test every three years
Age 30 and above: HPV test every five years if your results are normal
When to stop: Most women continue screening until around age 69 or 70, though your doctor can advise based on your individual health history
Screening is truly one of the most caring things you can do for your future self. If you’ve noticed any unusual changes, request an appointment with us to discuss whether cervical screening may be appropriate for you.
HPV vaccination: Your key step in preventing cervical cancer
Getting vaccinated reduces your risk of cervical, anal, and other HPV-related cancers. Even if you're already sexually active, the vaccine can still offer protection against strains you haven't been exposed to.
In Singapore, the HPV vaccine is included in the national immunisation programme, with structured schedules based on age:
Girls aged 9 to 17:
Two-dose schedule if under 15
Three-dose schedule if aged 15 or older
Adults aged 18 to 26 (and some up to age 45):
Three-dose schedule
Together with your doctor, you can find the timing that works best for your individual circumstances and health background. You'll find the HPV vaccine available at polyclinics, private clinics, and women's health centres across Singapore, so you can choose what feels most comfortable.
Ready to protect yourself? Schedule an appointment with Thomson Medical to discuss HPV vaccination with our team.
FAQ
Does everyone with HPV get cervical cancer?
Not at all. Most HPV infections clear naturally within one to two years without causing any problems. Only persistent high-risk HPV infections have the potential to lead to precancerous changes or cancer, and even then, regular screening can catch these changes early.
Can cervical cancer develop without HPV?
It's extremely rare. Nearly all cervical cancer cases are linked to HPV infection, which is why vaccination and screening are so effective at prevention.
How often should I get screened for cervical cancer?
In Singapore, it's recommended every three years for women aged 25 to 29 using a Pap test and every five years for women aged 30 and above using an HPV test. Your doctor can advise based on your individual health history.
How fast does cervical cancer spread if left untreated?
Without treatment, cervical cancer typically grows and spreads slowly over several years from the cervix to nearby tissues like the vagina, uterus, bladder, or rectum. More advanced cancer can spread more quickly, which is why early detection through screening is so valuable.
Can cervical cancer develop if I've had the HPV vaccine?
The vaccine protects against the most common high-risk HPV types, but not all of them. This is why regular screening remains important even after vaccination. Think of vaccination and screening as two layers of protection working together.
Can cervical cancer be cured if caught early?
Yes. When detected early, cervical cancer is highly treatable and often curable, typically through surgery or localised treatments. This is exactly why screening matters so much.
At what age is cervical cancer most likely to develop?
Cervical cancer most commonly develops in women between ages 35 and 44, though it can occur at any age after sexual activity begins. Starting regular screening from your mid-20s helps detect early changes long before cancer forms, giving you the best possible protection.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and advice based on your unique situation, request an appointment with Thomson Medical today.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) - Jurong:
6262 8588 (Call), 6262 8588 (WA) - Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
Notice
The range of services may vary between TWC/TS locations. Please contact your preferred branch directly to enquire about the current availability.
Request an Appointment