Noticing changes in your body can bring up questions and worries, especially when it comes to gynaecological health. Vaginal cancer is uncommon, but learning about its symptoms and risk factors can help you feel more confident and prepared.
Whether you are seeking reassurance about a symptom or learning more as part of routine health care, understanding vaginal cancer can help you make informed choices and feel supported in looking after your health.
What is vaginal cancer?
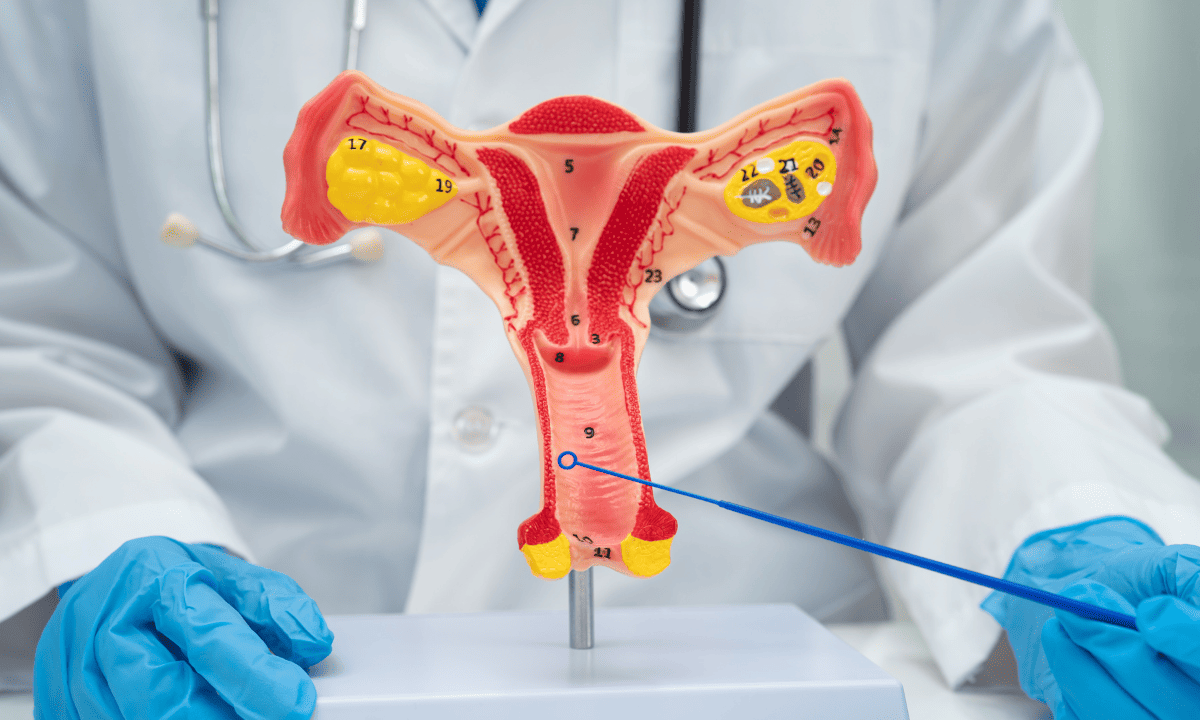
Vaginal cancer is a rare type of cancer that develops in the tissues of your vagina, the muscular birth canal connecting your uterus to the outside of your body.
Unlike cervical cancer, which starts in the cervix and is often detected through cervical cancer screening, vaginal cancer begins in the vaginal lining itself.
What causes vaginal cancer?
Vaginal cancer occurs when the normal cells in your vagina begin to grow uncontrollably, forming a tumour. While the exact cause is not always clear, certain factors can increase your risk if:
You are exposed to high-risk types of the human papillomavirus (HPV) (HPV 16 and 18)
You are over 60, although it can occur at any age.
You have had cervical or vulvar cancer before.
Your mother took diethylstilbestrol (DES) during her pregnancy.
You’ve had ongoing irritation or scarring in the vaginal area.
Types of vaginal cancer
There are several types of vaginal cancer. Although they all develop in your vagina, they begin in different kinds of cells, which means they can behave in different ways.
Squamous cell carcinoma:
The most common type.
It begins in the thin, flat cells that make up the surface lining of your vagina.
Adenocarcinoma:
A much rarer form.
It develops from glandular cells (cells responsible for producing fluids and natural secretions)
A specific subtype is vaginal adenocarcinoma, which has been linked to prenatal exposure to diethylstilbestrol (DES).
Vaginal melanoma:
A very rare and aggressive form that develops from pigment-producing cells (melanocytes) in the vaginal lining.
Vaginal sarcoma:
An uncommon type that arises from connective tissues such as muscle or supportive tissue within your vaginal wall.
Some women may also be diagnosed with vaginal intraepithelial neoplasia (VaIN). This isn’t cancer, but it means abnormal cells are present in the vaginal lining. If left untreated, VaIN can increase your risk of vaginal cancer over time.
Because vaginal cancer is rare, it’s easy to miss or mistake early symptoms for more common, less serious conditions. However, noticing changes and getting checked early can increase treatment options, improve outcomes, and help you feel more confident about your health.
What are the symptoms?
In the early stage, vaginal cancer may not cause noticeable symptoms. However, if you notice any of the following, it is important to speak to your doctor immediately:
Unusual vaginal bleeding, especially after sexual activity or after menopause
Persistent vaginal discharge that sometimes comes with a foul odor
Pain or discomfort during sexual intercourse
A lump or thickened area in your vaginal wall
Pelvic pain or urinary problems if your tumour presses on nearby organs
Even though these symptoms can be caused by less serious conditions, you’re encouraged to get them checked early to ensure that any problems are addressed before they progress.
If you have persistent symptoms, a history of HPV or related cancers, or want personalised advice based on your risk factors, schedule a consultation at Thomson Medical for a thorough assessment and supportive guidance on your next steps.
Our gynaecologic oncology specialist
Loading...
How is vaginal cancer diagnosed?
If your doctor is concerned about your vaginal cancer diagnosis, they will suggest a combination of tests to confirm your results and determine its extent.
Pelvic examination:
Your doctor will gently examine the vagina to check for anything that doesn’t look or feel normal.
Pap smear or HPV test:
These tests are usually performed to check for changes in the cervix.
Sometimes they can also spot unusual cells in your vagina.
Biopsy:
Your doctor takes a small sample of your vaginal tissue and analyses it under a microscope.
This is the only way to confirm whether you have cancer.
Imaging tests:
While waiting for answers can feel stressful or unsettling, together, these tests help your medical team build a clear picture of your diagnosis and choose the treatment approach that’s most appropriate for you.
Stages of vaginal cancer
Understanding the stage of your cancer helps you and your doctor make informed decisions about treatment. Staging simply describes how far the cancer has spread.
Vaginal cancer is usually grouped into four stages:
Stage I:
Cancer is only in the vaginal wall.
Stage II:
Cancer has spread to tissues surrounding the vagina but not the pelvic wall.
Stage III:
Cancer extends to the pelvic wall or nearby lymph nodes.
Stage IV:
Cancer has spread to nearby organs, such as the bladder or rectum, or to distant parts of the body.
Knowing the stage can feel overwhelming because it brings uncertainty about what comes next, but it helps your care team choose the safest and most effective treatment for you.
How is vaginal cancer treated?
Your treatment plan will be tailored to you, as it depends on several factors, including:
What type of vaginal cancer you have
The exact location of the tumour within the vagina
How advanced it is and whether it has spread
Your overall health
Your care team will design your treatment plan not only to remove or control the cancer but also to protect your quality of life and well-being.
Surgery
Your doctor may recommend surgery to remove the cancer while preserving as much normal vaginal function as possible. Depending on your situation, this may involve:
Local excision:
Your doctor will remove the tumour and a small area of healthy tissue around it.
Partial or total vaginectomy:
Part or all of your vagina may be removed if your tumour is larger or more extensive.
Lymph node removal:
Your doctor may check nearby lymph nodes to analyse your cancer spread.
It is normal to feel sore or swollen after surgery, and the vaginal area may feel different while it heals. Your care team will support you through this and help you stay as comfortable as possible during recovery.
Radiation therapy
Radiation therapy (radiotherapy) uses high-energy rays to treat cancer cells. Your doctor may recommend it on its own or after surgery, depending on what is best for your situation.
There are two main types of radiotherapy. External beam radiotherapy directs radiation at the cancer from outside your body, while brachytherapy places radiation close to your tumour so it can be treated more precisely.
Chemotherapy
Chemotherapy uses medicines to treat cancer cells throughout your body. If vaginal cancer is more advanced, your doctor may recommend chemotherapy alongside radiotherapy, as the two treatments can work better together.
To allow your body time to rest and recover between sessions, your doctor will spread out the treatment over several weeks. The main goal is to make sure you feel supported and safe during treatment.
Targeted therapy and immunotherapy

In some situations, these therapies work by blocking signals that cancer cells need to grow or by strengthening your immune system’s ability to recognise and destroy cancer cells.
They are not suitable for everyone but may be considered if standard treatments are less effective or if a more targeted approach is needed.
If you are exploring treatment options, have been diagnosed, or want a care plan tailored to your health, schedule a consultation at Thomson Medical to receive clear guidance and a thorough discussion of the most suitable next steps for you.
How to prevent vaginal cancer
Although vaginal cancer cannot always be prevented, there are steps you can take to reduce your risk:
Get HPV vaccination, as it offers you protection against high-risk HPV types
Attend regular screenings, including Pap tests, HPV tests, and cancer screenings, to detect abnormal changes early
Avoid unhealthy lifestyle habits such as smoking
Address any abnormal Pap smear results, persistent infections, or previous gynaecological cancers promptly
If you want to learn more about HPV vaccines or routine screenings, schedule a consultation at Thomson Medical for guidance tailored to you.
FAQ
Is vaginal cancer the same as cervical cancer?
No, they are different. Vaginal cancer starts in the lining of your vagina, while cervical cancer begins in the cervix, which sits at the lower part of your uterus. You might see similarities in symptoms or treatments, but the origin and behaviour of each cancer are not the same.
Can vaginal cancer return after treatment?
Sometimes, yes. This can feel worrying but recurrence is not uncommon in many cancers, which is why your follow-up care matters so much. Regular check-ins are there to protect you, catch any changes early, and give you the best chance of responding quickly if needed.
Is vaginal cancer caused by HPV?
HPV is one of the most significant risk factors, especially for the squamous cell type. Most HPV infections do not lead to cancer, and many clear on their own, but persistent high-risk strains can increase your risk over time. Vaccination and screening are helpful ways to protect yourself.
Can vaginal cancer be cured completely?
Yes, it can be, particularly when found early. Some women will reach complete remission, meaning no detectable cancer remains after treatment. Your outcome depends on factors like stage and cell type, but successful treatment and long-term cancer-free results are absolutely possible for many women.
What is the survival rate of vaginal cancer?
Survival rates vary based on how early the cancer is diagnosed. When it is caught at an early stage, outcomes tend to be much more favourable. For later stages, combined treatments may be needed. Your doctors can give you the most accurate estimate based on your personal diagnosis, and they will support you in understanding it clearly.
Will treatment affect my fertility or intimacy?
Some treatments may affect fertility or intimacy, depending on what is safest for you. This can include:
Fertility:
Chemotherapy may temporarily affect your ovarian function, which can impact your menstrual cycle or fertility in some cases.
Intimacy comfort:
Radiotherapy or surgery may cause side effects such as dryness, sensitivity, or tightening of vaginal tissue.
Your care team will guide you through every option so you feel informed, supported, and confident in your journey.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice based on your unique situations, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) - Jurong:
6262 8588 (Call), 6262 8588 (WA) - Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
Notice
The range of services may vary between TWC/TS locations. Please contact your preferred branch directly to enquire about the current availability.
Request an Appointment