Dealing with recurring yeast infections can be uncomfortable and frustrating, and it is natural to wonder whether frequent symptoms might be linked to something more serious. Many people quietly worry about what these repeated infections could mean for their long-term health.
The good news is that yeast infections themselves are usually not linked to cervical cancer. Understanding why they occur, how they differ from cervical cancer, and when to seek medical advice can help put your mind at ease and guide you towards the right care.
Yeast infection and cervical cancer: Is there a connection?
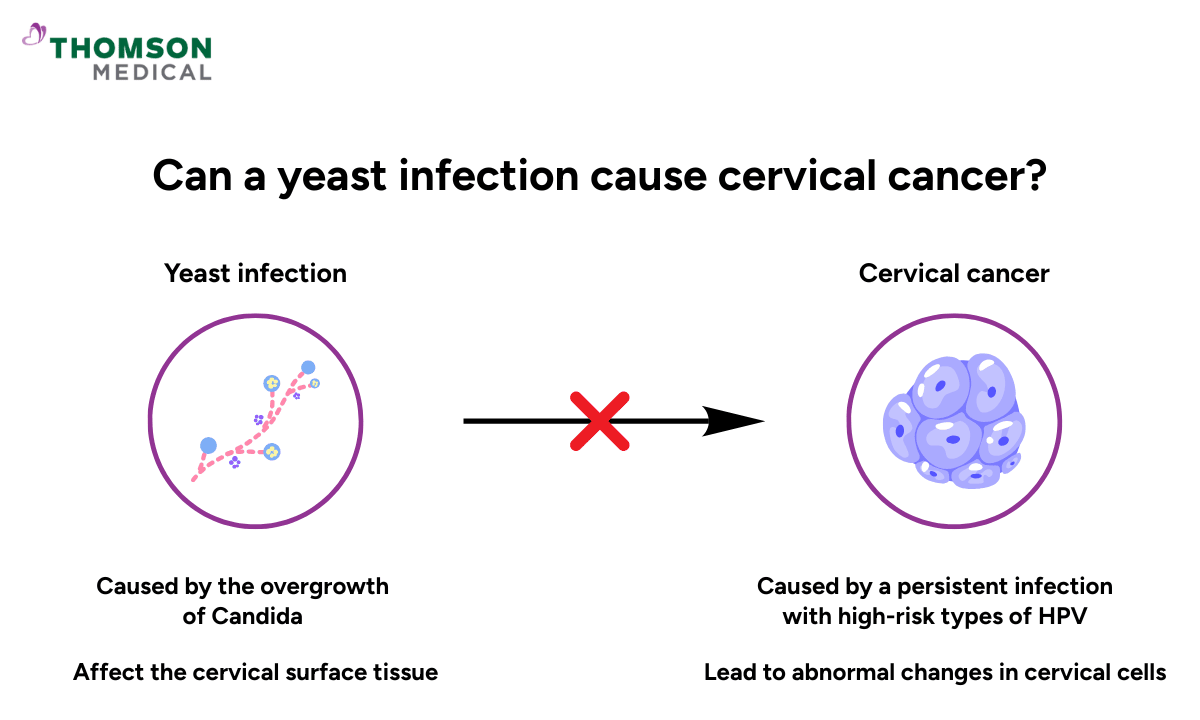
Yeast infections and cervical cancer are two different conditions.
Yeast infections happen when Candida (a fungus that's normally in your vagina) starts growing too much. It's annoying and itchy, but it only affects the surface tissue. Antifungal medication usually clears it right up.
Cervical cancer, on the other hand, develops in the cervix and is most commonly caused by a persistent infection with high-risk types of human papillomavirus (HPV). Over time, HPV can lead to abnormal changes in cervical cells, which may progress to cancer if left undetected.
Here's the key thing: yeast infections don't cause those cell changes. They just don't work that way. So even if you've had yeast infections multiple times, that doesn't raise your cervical cancer risk at all.
Causes of yeast infections
Once you know that a yeast infection doesn’t lead to cervical cancer, you may start to have more questions: Why does this keep happening to me? And why does it come back again and again?
It comes down to balance. Your vagina has its own ecosystem – good bacteria and a bit of yeast living alongside each other.
What often surprises people is that yeast isn’t the enemy. Yeast plays an important role in keeping your vaginal environment dynamic and resilient. Its presence encourages healthy bacteria while helping your immune system stay active and responsive. In this way, yeast becomes part of the system that helps your vagina adapt to hormonal shifts, stress, and everyday life.
When everything's in harmony, you're fine. But when something throws that balance off, the yeast takes over. That's when you get issues such as vaginal itching, burning, irritation, or that cottage cheese-like discharge.
This imbalance isn’t a sign that you’ve done anything wrong. Many everyday situations can tip the scales without you even realising it, such as:
Antibiotic use:
This medication can reduce protective vaginal bacteria.
Hormonal changes:
During pregnancy, menopause, or different phases of your menstrual cycle, hormonal changes may affect the natural balance inside your vagina.
Uncontrolled diabetes:
When blood sugar is consistently high, yeast infections tend to happen more often and can be harder to clear.
Tight or non-breathable clothing:
These types of clothing may trap warmth and moisture – an environment yeast thrives in.
A weakened immune system:
Even temporarily, a weakened immune system makes your body unable to control the overgrowth of Candida.
Stress:
Stress may affect your body’s ability to regulate itself.
Diet:
Higher sugar levels can encourage yeast growth.
Sexual activity:
You may have a yeast infection after sexual intercourse, as sexual activity can alter the vaginal environment.
If you’ve been dealing with recurrent yeast infections, it doesn’t mean your body is failing you. It could simply mean that one or more of these factors keeps nudging your vaginal balance out of place.
If something doesn’t feel quite right or symptoms keep coming back, schedule an appointment with Thomson Medical. Our O&G specialists will help you understand what’s happening and gently restore your vaginal health with a personalised care plan.
Our O&G specialist
Loading...
What to do if you have a yeast infection

If you think you have a yeast infection, you can grab an over-the-counter antifungal cream or suppository from the pharmacy. Most women start feeling better within a few days.
But if it keeps coming back, or the treatment just isn't working, it’s important to consult your doctor. This is because other conditions, such as different vaginal infections or sexually transmitted infections (STIs), can cause similar symptoms and may need a different approach.
In the meantime, there are some simple things you can do to keep your vaginal health in check and reduce the chances of future infections:
Wearing breathable, cotton underwear
Use antibiotics only when truly necessary
Maintain gentle vaginal hygiene
Yeast infection is a common experience for many women. With the right care and a little patience, symptoms usually improve and become easier to manage over time.
Causes and risk factors of cervical cancer
So if yeast infections aren't the culprit, what actually causes cervical cancer?
The answer is HPV. About 85% of sexually active people will come across it at some point in their lives. Luckily, your body usually clears it on its own without you even realising.
Cervical cancer only happens when a high-risk type of HPV sticks around for years. Over that time, it slowly causes changes in the cells of your cervix. If those changes aren't caught early, that's when cancer can develop.
Some factors can make it harder for your body to clear HPV or increase the chance that these cell changes go unnoticed, such as:
Smoking
A weakened immune system
Having multiple sexual partners
Early sexual activity
Lack of access to routine screening, including Pap smears and HPV tests
It’s important to remember that having one or even some of these risk factors does not mean you will develop cervical cancer. They simply help explain why regular cervical cancer screening, HPV vaccination, and early medical care play such an important role in prevention.
Whether you’re concerned about HPV, cervical cancer risk, or your screening, schedule an appointment with Thomson Medical. Our O&G specialists will help you understand your options and take the next step with confidence.
FAQ
Can a yeast infection cause an HPV-positive result?
No, yeast infections are caused by Candida species. They do not cause HPV infection or a positive HPV test result.
Is Candida spp. normal on a Pap test?
Candida species are normally present in small amounts in your vagina, and a Pap smear may occasionally detect them. Their presence on a Pap smear does not indicate cancer.
Is Candida spp. an STI?
No, Candida is not considered a sexually transmitted infection (STI). While sexual activity can sometimes contribute to irritation or changes in vaginal flora that trigger yeast overgrowth, Candida naturally exists in your body. Yeast infections can also occur in women who are not sexually active.
Can untreated yeast infections cause other serious health problems?
In most healthy women, yeast infections are not severe. Rarely, untreated severe yeast infections can spread in people with weakened immune systems, such as those with HIV, diabetes, or patients undergoing chemotherapy, potentially leading to systemic infections.
What causes 90% of cervical cancer?
About 90% of cervical cancer cases are caused by persistent infection with high-risk types of HPV, most commonly HPV types 16 and 18.
What are the symptoms of cervical cancer?
Early cervical cancer may not cause any symptoms. When symptoms do appear, they may include:
Abnormal vaginal bleeding (such as bleeding after sex or between periods)
Unusual vaginal discharge
Pelvic pain, or pain during intercourse
These symptoms are not specific to cervical cancer and can be caused by other conditions. If you notice any of them, it’s best to consult your doctor promptly.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and advice based on your unique situation, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) - Jurong:
6262 8588 (Call), 6262 8588 (WA) - Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
Notice
The range of services may vary between TWC/TS locations. Please contact your preferred branch directly to enquire about the current availability.
Request an Appointment