If you've already been through cervical cancer once, it is natural to feel worried about the possibility of it returning. Many women have questions about why recurrence happens and what steps they can take to reduce this risk.
Knowing when recurrence is most likely, how it is monitored, and what treatment options are available can help you feel more prepared and supported. With the right information and medical care, you can focus on taking each step forward with greater confidence and reassurance.
What cervical cancer recurrence means
Recurrence means that your cervical cancer has returned after treatment and a period when no cancer could be detected.
Recurrence can happen in three ways:
Local recurrence, where cancer returns in or near your cervix or top of your vagina.
Regional recurrence, which means cancer spreads to nearby lymph nodes or pelvic tissues.
Distant recurrence, where cancer cells travel to organs such as your lungs, liver or bones.
This happens because some cancer cells may be too small to detect during treatment or may have already spread before treatment began. These cells can stay dormant for months or even years before growing large enough to be found on scans or tests.
The type of recurrence influences which treatment approach may work for you. If you're feeling worried about the road ahead, know that regular follow-up appointments are there to support you – they help your doctor catch any signs of recurrence early, when treatment tends to work more effectively.
When cervical cancer may return
The first two to three years after treatment need the closest attention as this is when most recurrences occur. It's natural to feel concerned during this period, which is why you'll see your doctor more regularly (usually every three to six months). These frequent visits are designed to catch any changes early and give you peace of mind.
After going through this period with clear results, you can take some comfort knowing your risk gradually decreases. Your appointments may then be spaced further apart, normally between every 6 to 12 months.
While late recurrences past five years are uncommon, they can occur with certain cancer types. This is why maintaining your follow-up care matters, even years later when everything feels stable.
While it may be tiring to keep attending appointments even when you're feeling fine, these check-ins remain an important part of your long-term care.
Your doctor will tailor your monitoring schedule based on your cancer stage, treatment approach, and what your specific situation calls for.
Factors that may increase recurrence risk
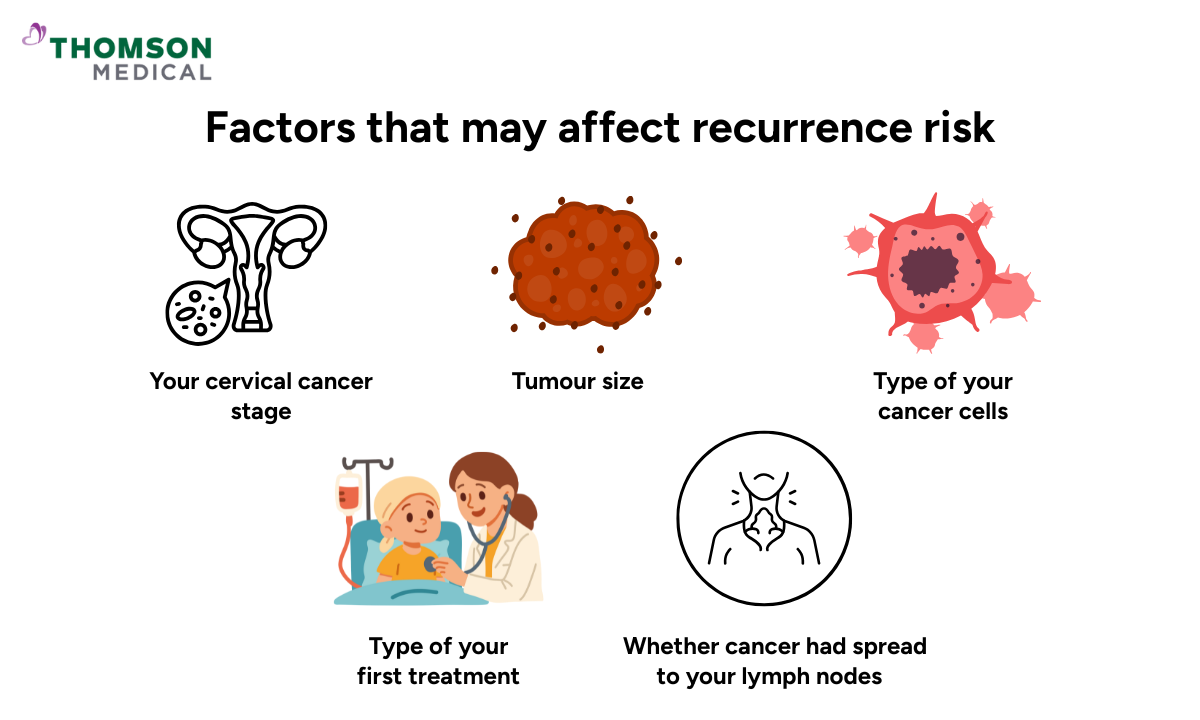
Every woman's experience with cervical cancer is unique, and so is her path after treatment. Some factors may mean you'll need closer monitoring, which helps your doctor plan the right follow-up care for you.
Stage and tumour size at diagnosis
The stage of your cervical cancer when first diagnosed is one of the strongest indicators of recurrence risk:
Early-stage (Stage I):
If you had early-stage cancer, recurrence rates are lower, around 5 to 15%.
Locally advanced (Stages II to III):
Locally advanced cancers have a moderate to high risk, approximately 20 to 40%.
Stage IV:
Stage IV cancers have a higher recurrence or persistence risk, over 50%.
Tumour size also plays a role. If your tumour was larger than 4 cm, there's a higher chance of recurrence, as larger tumours are more likely to have spread tiny cancer cells to nearby tissues before treatment began.
The type of your cancer cells matters as well. Poorly differentiated tumours (where cancer cells look very different from normal cells) and adenocarcinoma types tend to recur slightly more often than squamous cell cancers.
These numbers reflect what happens on average across many women, but they don't predict your individual journey. What matters just as much as your diagnosis is how your cancer was treated and how your body has responded since then.
How your first treatment affects recurrence risk
The type and completeness of your initial cervical cancer treatment affect your recurrence risk. If you had surgery, clear margins (no cancer cells at the edges of removed tissue) reduce your risk. Incomplete margins can increase the chance of recurrence.
Radiation therapy and chemotherapy work well at reducing recurrence, though they can't eliminate risk completely. Following your full treatment plan gives you the best chance of staying cancer-free.
Cancer that has spread to your lymph nodes also increases recurrence risk. The more lymph nodes affected, the higher the risk.
Other factors that can influence recurrence include:
Persistent HPV infection after treatment
Smoking, which weakens your body's ability to fight cancer cells
A weakened immune system from conditions such as HIV or long-term medication use
Your doctor will consider all these factors when planning your follow-up care. While it can feel overwhelming to think about all these risk factors, knowing them helps you and your care team stay alert and respond quickly if needed.
If you're concerned about your recurrence risk or would like to understand how these factors apply to your situation, schedule an appointment with Thomson Medical. Our doctors can review your treatment history and help you understand what to watch for during your recovery.
Symptoms that may signal cervical cancer recurrence
Being familiar with what to watch for can help you catch recurrence early. These symptoms don't always mean cancer has returned, but it's worth mentioning them to your doctor.
Key symptoms include:
Abnormal vaginal discharge or bleeding
Persistent pelvic, lower back or abdominal pain
Pain during sexual intercourse
Leg swelling or pain on one side
Unexplained weight loss or loss of appetite
Ongoing fatigue that doesn't improve with rest
Persistent cough or shortness of breath
If any of these symptoms last more than a week or two, get in touch with your doctor. Trust your instincts – if something feels wrong, don't wait until your next scheduled appointment.
Sometimes recurrence happens without any noticeable symptoms. This is why your follow-up appointments matter so much – they give your doctor a chance to spot changes early, even when you're feeling fine. You don't need to worry about missing something on your own.
Cervical cancer specialists in Singapore
Loading...
How your doctor monitors for recurrence
Regular follow-up care is one of the most effective ways to catch recurrence early. Your doctor will create a schedule based on your individual risk factors.
Your doctor may use several tests to check for recurrence, such as:
Pelvic exam and Pap test to look for local recurrence
HPV testing to detect persistent infection
Imaging studies such as MRI scans, CT scans or PET scans to check any changes in your body
Biopsy of any suspicious tissue to confirm whether cancer has returned
If you notice anything new or unusual between appointments, let your doctor know. Don’t be afraid to reach out – your observations about your own body are valuable, and catching any changes early means you'll have more treatment options available to you.
What to expect if cervical cancer returns
.png?branch=production)
Learning that cancer has returned can feel devastating. You may feel angry, scared or simply exhausted at the thought of more treatment. These feelings are completely normal, and the good news is that you don't have to navigate this on your own.
The location of the cancer will affect what treatments are recommended. Local recurrences may respond well to surgery or radiation, while distant recurrences usually need systemic treatments such as chemotherapy or immunotherapy. Your previous treatments and current health also shape which options make sense for you.
Your doctor may recommend these approaches:
Surgery:
For isolated local recurrences, surgery may remove the cancer.
Radiation therapy:
If you haven't had radiation before, it can work well. In some cases, re-irradiation may be possible.
Chemotherapy:
Cisplatin-based regimens are commonly used to slow cancer growth.
Targeted therapies:
These therapies use medications that target specific aspects of cancer cells to help control their spread.
Immunotherapy:
Immunotherapy helps your immune system recognise and fight cancer cells.
Your doctor will talk through the benefits and potential side effects of each option with you. Take your time to ask questions and consider what feels right for your situation. With the right support and information, you can move forward knowing you're making the best choices for your long-term health.
If you've been told your cancer has recurred and feel unsure about your next steps, schedule an appointment with Thomson Medical. Our doctors can explain your treatment options and work with you to create an approach that fits your health needs.
FAQ
How common is cervical cancer recurrence after treatment?
About 10 to 30% of patients experience recurrence, depending on the original cancer stage and treatment received. Early-stage cancers have lower recurrence rates than advanced stages.
How soon after treatment can cervical cancer come back?
Most recurrences happen within the first 2 to 3 years after treatment, though late recurrences can occur even after 5 years.
Can cervical cancer recurrence be detected before symptoms appear?
Yes. Regular follow-up appointments, pelvic exams, and imaging tests can detect recurrence before you notice any symptoms. This is why keeping your scheduled appointments is so important.
Is recurrent cervical cancer curable?
It depends on where the cancer has returned. Local recurrences may be curable with surgery or radiation. Regional or distant recurrences are more challenging to cure, but treatments can control the cancer and improve your quality of life.
How often should I have follow-up appointments after treatment?
Usually every 3 to 6 months for the first two years, then every 6 to 12 months up to five years. Your doctor will adjust this schedule based on your individual risk.
What can I do to lower my risk of recurrence?
Attend all follow-up appointments, quit smoking, maintain a healthy lifestyle with regular exercise and a balanced diet, and report any unusual symptoms promptly to your doctor.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice based on your unique situations, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
.png%3Fbranch%3Dprod&w=3840&q=75)