Many women start to think about ovarian cancer as they notice changes in their bodies or move into new stages of life. You might find yourself wondering whether your age puts you at higher risk, or whether certain symptoms should be taken more seriously.
Ovarian cancer is most commonly diagnosed after menopause, with most cases occurring in women over the age of 50. That said, age is only one part of the picture. Understanding how risk changes over time, which types of ovarian cancer are seen at different ages, and when it is worth speaking with your doctor can help you stay informed without unnecessary worry.
What are the early symptoms of ovarian cancer?

It's natural to worry about ovarian cancer, as it can be hard to predict and catch early.
In its early stages, ovarian cancer often causes vague symptoms deep in your pelvis. They're easy to miss or blame on digestion or hormonal shifts.
Some early warning signs may include:
A persistently swollen abdomen
Ongoing abdominal or pelvic pain
Feeling bloated more often than usual
Changes in your bowel movements, such as constipation or diarrhoea
Nausea or feeling unwell
Loss of appetite or feeling full quickly
Needing to urinate more often
These symptoms do not always mean cancer, but if they're new, won't go away, or are getting worse, it’s important to get them checked.
Who is at higher risk of developing ovarian cancer?
There are several types of ovarian cancer, such as epithelial ovarian cancer (the most common), fallopian tube cancer, germ cell ovarian cancer, and sex cord stromal tumours.
The risk factors below apply mainly to epithelial ovarian cancer. They don't necessarily apply to rarer types like germ cell or stromal tumours.
Factors that may increase your risk include:
Getting older
Inherited BRCA mutations (BRCA1, BRCA2 genes) or Lynch syndrome
Starting your period before age 12
Going through menopause after age 52
Not having children
Past radiation treatment to your pelvis
Endometriosis (when tissue like your uterine lining grows outside your uterus)
Having one or more of these risk factors doesn't mean you'll get ovarian cancer. But it might mean more regular check-ups or earlier testing could help.
If you recognise any of these risk factors and feel unsure about what they mean for you, you don’t have to figure it out on your own. Request a consultation at Thomson Medical, where our O&G specialists can help assess your individual risk and discuss whether closer monitoring or genetic counselling is appropriate.
Our ovarian cancer specialist
Loading...
How to diagnose ovarian cancer early
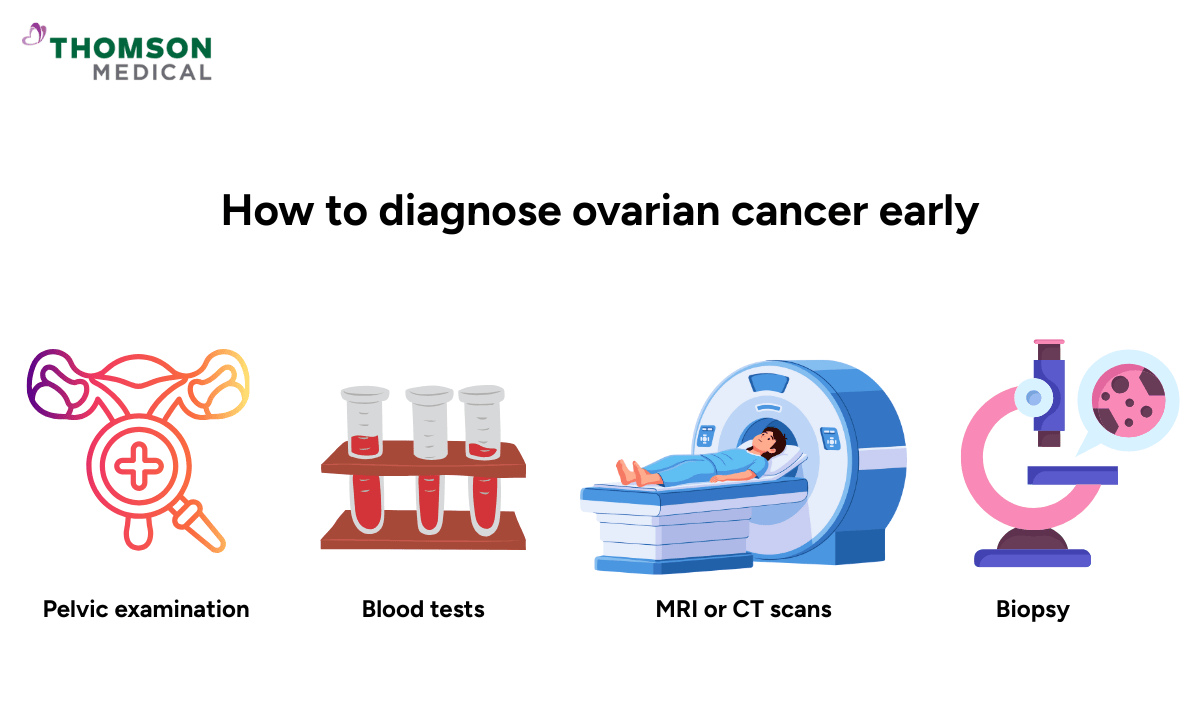
Because there's no single screening test for ovarian cancer, diagnosis often involves a step-by-step process. Your doctor might use a physical exam, blood tests, and imaging to get a full picture.
Pelvic examination
A pelvic exam is usually the first step. On its own, this exam might not catch very small tumours, but it helps your doctor decide if you need more tests.
Your doctor gently presses on your abdomen and does an internal vaginal exam to check the size, shape, and position of your womb and ovaries. This pelvic exam might feel a bit uncomfortable, but it shouldn't hurt and is usually quick.
If you're having your first pelvic exam, it's normal to feel nervous about it. The exam happens in a private room, and your doctor will explain what they're doing before they start. You can always request the test to stop if you're anxious, need a break, or have questions.
Blood tests
You might have a blood test called CA125, which measures a protein that can be high in ovarian cancer. The test is a simple blood draw and is usually quick and painless.
It’s important to know that CA125 levels can also go up because of things that aren't cancer, like your period, endometriosis, or ovarian cysts. And in some early-stage ovarian cancers, CA125 stays normal.
That's why your doctor looks at this test alongside imaging results, not on its own.
MRI scan
An MRI scan is a non-invasive imaging test that allows your doctor to see your ovaries in detail. MRI scans are helpful in distinguishing harmless cysts from growths that need a closer look. They’re usually recommended after something shows up on an ultrasound or you have symptoms, not as a first test.
During the scan, you lie on a table that slides into the MRI machine. It doesn't hurt and doesn't use radiation. You'll hear loud knocking or humming sounds while it's running.
If you don't like enclosed spaces, let the staff know. They can see and hear you the whole time, and you can talk to them whenever you need to.
CT scan
A CT scan shows what's happening inside your body. It's often used to check the size of an ovarian mass and see if anything has spread to nearby organs or lymph nodes.
The scan is quick and doesn't hurt. You lie on a table that moves through the scanner, and the whole thing takes just a few minutes.
Sometimes you'll get a contrast dye through an intravenous to make the images clearer. This might give you a brief warm feeling or metallic taste, but it goes away fast.
Biopsy
A biopsy is a procedure to remove a piece of tissue or a sample of cells from your body so that it can be tested in a laboratory. It is the only way to confirm ovarian cancer. The word "biopsy" can sound scary, but how it's done depends on your situation.
In most cases, a biopsy happens during surgery, either through laparoscopic surgery or open surgery. You'll be under general anaesthesia, so you'll be asleep and won't feel anything. This means you need to be admitted to hospital for a few days.
Sometimes, a biopsy can be done using CT or ultrasound imaging to guide it. This is less invasive and might use local anaesthesia with light sedation. Some patients go home the same day while others stay briefly for observation.
Before any biopsy, your doctor will explain why you need it, how they'll do it, what type of anaesthesia you'll have, and what recovery looks like. You'll have time to ask questions and discuss any concerns so that you feel informed and supported.
When should you see a doctor?
There's no routine screening test for ovarian cancer but catching symptoms early matters. Here's what to look for and when to get help.
See a doctor if you have symptoms that last more than two weeks, including:
Abdominal or pelvic pain
Bloating
Less appetite
Changes in your bowel movements or urination
If ovarian or breast cancer runs in your family, it’s best to talk to your doctor sooner.
Ovarian cancer symptoms are vague and easy to confuse with other things. If something feels off in your body, get it checked. That's not overreacting; it's looking after yourself.
Trust your body. When symptoms don’t feel right or don’t go away, seeking medical advice can offer clarity and peace of mind. Request a consultation with our O&G doctors at Thomson Medical, where your concerns are listened to and your care is tailored to you.
FAQ
Can ovarian cancer be detected early with regular check-ups?
Ovarian cancer is difficult to detect early with routine check-ups, as the ovaries are located deep in your pelvis and often cause no symptoms in early stages. Early detection relies mainly on recognising symptoms and seeking regular gynaecological care.
What is the most reliable test for early ovarian cancer detection?
There is no single reliable test for early detection of ovarian cancer. Tests such as CA-125 blood tests and transvaginal ultrasound may be used for women at high risk, but they are not recommended as routine screening tools for everyone.
Does a normal CA-125 test mean I’m cancer-free?
A normal CA-125 level does not rule out ovarian cancer, especially in early stages. Some ovarian cancers do not raise CA-125 levels, while several non-cancerous conditions can cause CA-125 to be elevated.
How often should I get screened if I have a family history?
If you have a family history of ovarian or breast cancer, it’s best to consult your doctor. They may recommend screening with CA-125 blood tests and transvaginal ultrasound every 6–12 months, starting around age 30–35 or earlier, depending on your family history.
Can lifestyle changes lower the risk of ovarian cancer?
A healthy lifestyle may help lower your risk of ovarian cancer. These include:
Maintaining a healthy weight
Eating a balanced diet rich in fruits and vegetables
Avoiding smoking
Limiting alcohol intake
What is the difference between an ovarian cyst and ovarian cancer?
Ovarian cysts are common, usually harmless, fluid-filled sacs that often resolve on their own. Ovarian cancer involves abnormal growth of malignant cells, often forming solid or complex masses. While symptoms can overlap, cancer is much rarer and requires imaging tests and sometimes a biopsy for diagnosis.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and advice based on your unique situation, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
For more information, contact us:
Thomson Fertility Centre
- Paragon: 6252 7766
Thomson Specialists (Women's Health)
Thomson Women's Clinic
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
