It's the day after you had intercourse with your significant other, and when you go to the bathroom, you notice blood on your underwear. Seeing this, you might feel worried and confused. What is this bleeding? What's causing it? Is it serious?
The good news is that bleeding after sex is common and is usually caused by something mild. To help ease your worries, let's look at what might be causing this bleeding and when you need to see a doctor.
What is bleeding after sex?
Bleeding after sex, also known as postcoital bleeding, is light bleeding that occurs following sexual intercourse. However, bleeding may also occur when you're in the middle of the action. It can be caused by various factors, ranging from vaginal dryness to more serious health conditions such as polyps or fibroids.
While some women do experience bleeding during or after intercourse, it should always be evaluated by a doctor to rule out underlying conditions. This is particularly important if the bleeding occurs consistently or is accompanied by other symptoms.
What causes bleeding after sex?
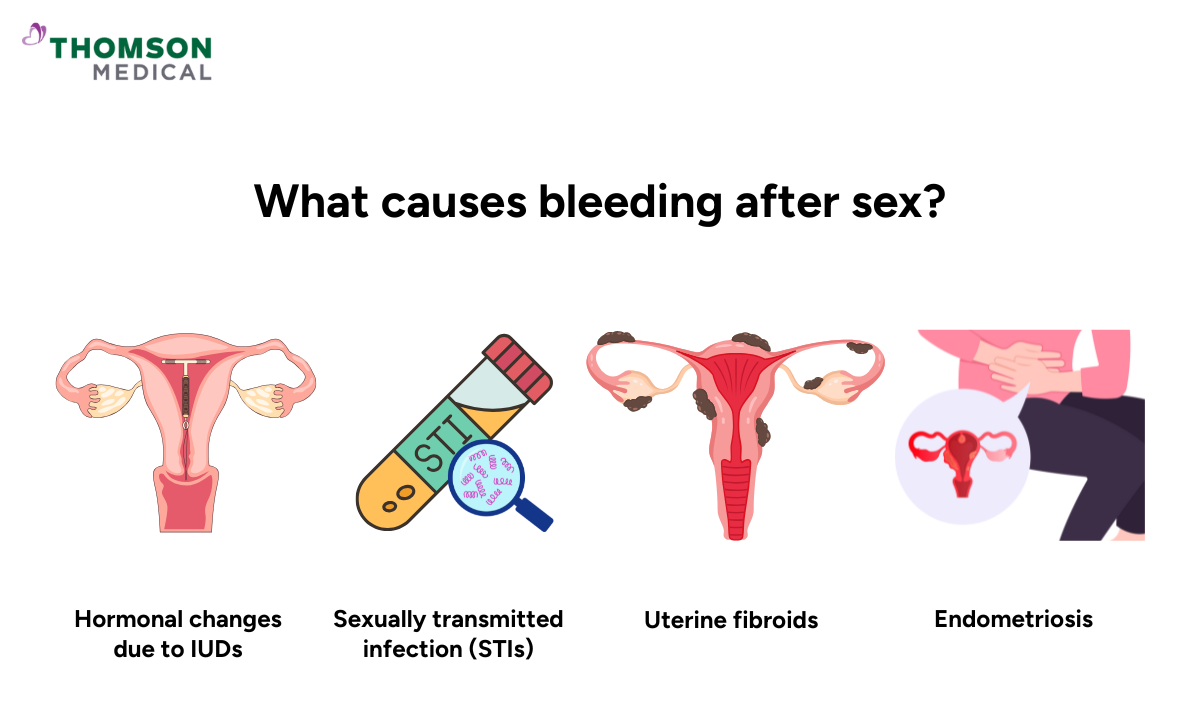
There are various factors that can cause vaginal bleeding during or after intercourse. Even though most of these causes are mild, postcoital bleeding might need medical attention in some cases. The most common causes are:
Vaginal dryness
Vaginal dryness occurs when there isn't enough natural lubrication in the vagina. This symptom is common if you aren’t aroused enough before intercourse, if you are currently breastfeeding, or if you are in menopause.
Without adequate lubrication, friction during sexual intercourse can cause small tears in the vaginal tissue, leading to bleeding and making it uncomfortable or painful.
Minor vaginal or cervical injury
If you and your partner have rough or vigorous intercourse, it can cause cuts or bruising to the vaginal wall or cervix (the lower part of the womb), which can lead to postcoital bleeding. Usually, these injuries heal quickly without any complications.
Infections
Infections can cause inflammation of the cervix or vaginal tissues, making them more prone to bleeding.
This includes sexually transmitted infections (STIs) such as chlamydia, herpes, trichomoniasis, or gonorrhoea as well as vaginal infections like yeast infections or bacterial vaginosis.
Endometriosis
Endometriosis is a condition where tissue similar to that which lines the womb grows outside of it. This can cause pain and bleeding during or after intercourse.
Cervical polyps and fibroids
Cervical polyps and uterine fibroids are abnormal growths that can also cause bleeding.
While these are usually non-cancerous, they may require treatment if they cause persistent symptoms.
Hormonal changes
Hormonal changes due to contraceptives such as pills or intrauterine devices (IUDs) can cause postcoital bleeding to occur more frequently, especially during the first few months of use.
Additionally, hormonal changes that happen during perimenopause (the transition phase before menopause) or menopause can also make the vagina dry.
When oestrogen levels go down, the body makes less cervical mucus, and the vaginal walls become thinner, which makes it more likely that the vagina will tear and cause bleeding.
Other medical conditions
Pelvic inflammatory disease (PID) is an infection of the reproductive organs that can damage tissue and cause irregular bleeding.
Medications such as blood thinners or anticoagulants (e.g. warfarin or heparin) can increase the risk of bleeding during or after intercourse.
In rare cases, bleeding after sex can be a sign of cervical cancer.
Are there any risk factors that make bleeding after sex more likely?
Besides the previously mentioned causes of postcoital bleeding, the following risk factors increase your likelihood of experiencing such bleeding:
Having unprotected intercourse or multiple sexual partners increases the risk of infections such as chlamydia or gonorrhoea.
Having conditions such as diabetes or thyroid disorders, which may affect vaginal tissue health.
Having cervical or uterine polyps, or in rare cases, cervical, vaginal, or uterine cancer.
Using vaginal douches or perfumed products can irritate or disrupt the natural balance of the vagina.
Recently given birth or are breastfeeding, where hormonal changes might make the vaginal walls more delicate.
If you occasionally experience minor bleeding, it’s usually nothing to worry about. However, if you experience regular bleeding after intercourse, it’s recommended that you seek medical help to rule out infection or anything more serious.
As bleeding after sex can have many possible causes, a proper medical assessment is the only way to determine the exact reason. For further information or to discuss your concerns, schedule an appointment with Thomson Women's Clinic.
Our sexual health specialist
Loading...
When should you seek medical help?
In most cases, light bleeding during or after sexual intercourse is usually not a cause for concern, especially if it happens occasionally. However, you should seek medical attention if you experience any of the following symptoms:
Fever
Severe abdominal pain
Dizziness or light-headedness
Pelvic pain or pain when urinating
Regular or recurrent vaginal bleeding
Bleeding after sex, although you’re menopausal
Heavy or persistent bleeding that lasts for more than a few days
Abnormal vaginal discharge, such as a foul-smelling, yellowish, or green colour
If you haven't had your period in a while and are bleeding from your vagina alongside stomach pain, these symptoms could be a sign of an ectopic pregnancy. Because this is a serious condition, it’s recommended that you seek immediate medical attention.
How does the doctor diagnose vaginal bleeding after sex?
Your doctor will first ask you about your symptoms and medical history to figure out what is causing your postcoital bleeding. This helps them determine when and how the bleeding occurs, its severity, and what other factors might be involved. They may ask whether:
You’ve experienced any heavy or irregular periods
You’ve had any bleeding disorders or take blood-thinning medication
You’ve recently started taking birth control pill or changed contraception methods
You experience pain during sex, which may suggest vaginal dryness, inflammation, or infection
You have any other symptoms, such as abnormal vaginal discharge, pelvic pain, or pain when urinating
Your doctor may also carry out some examinations or tests, which can include:
Pelvic examination to look for signs of cervical ectropion, infection, inflammation, cervical or vaginal polyps, or uterine prolapse.
Swab tests to check for sexually transmitted infections (STIs) such as chlamydia, trichomoniasis, or gonorrhoea.
Pap test, to collect a small sample of cells from the cervix to look for abnormal or precancerous changes.
An ultrasound scan, such as a pelvic or transvaginal ultrasound, can be performed to help identify fibroids, polyps, or other structural issues in the womb or cervix.
If your Pap test results are abnormal, your doctor may recommend a colposcopy, where they can take a small tissue sample (biopsy) for testing.
An endometrial biopsy may be performed if you're postmenopausal or have risk factors such as persistent bleeding or thickened endometrium on ultrasound
The tests your doctor suggests will depend on how old you are and what symptoms you’re experiencing. In most cases, once the underlying problem is found, the cause of postcoital bleeding can be managed.
How is bleeding after sex treated?
Since there’s no single cause of postcoital bleeding, the treatment depends on the underlying cause.
Infections:
Antibiotics treat bacterial infections such as chlamydia, gonorrhoea, or bacterial vaginosis.
Antifungal medications are used to treat yeast infections.
Hormonal treatments:
If bleeding is related to hormonal fluctuations or contraceptive use, your doctor may suggest adjusting your birth control method or prescribing hormone therapy.
Polyps or fibroids:
Cervical polyps can be removed through a procedure called polypectomy.
Depending on their severity, fibroids may require surgical removal, such as a myomectomy or hysterectomy (removal of the uterus).
Vaginal dryness:
If you experience persistent dryness, especially related to menopause, low-dose vaginal oestrogen therapy in the form of creams, tablets, or rings can help restore moisture.
Other treatments:
In rare cases, conditions such as endometriosis or cervical cancer may require more extensive surgical treatment or cancer therapy.
If you're experiencing bleeding after sex, schedule an appointment with Thomson Women's Clinic. Our specialists can help assess your condition, determine its underlying causes, and provide personalised treatment in a private setting.
How to prevent postcoital bleeding?
Depending on what is causing the bleeding, there are different preventative measures. However, the following general prevention methods are recommended:
Use water-based lubricants before intercourse to reduce friction
Allow adequate time for foreplay before penetration
Avoid scented or harsh feminine hygiene products
Practise safe sex with protection and get regular STI screenings
Use a vaginal moisturiser every two to three days if you experience regular dryness
Talk to your partner to ensure that you both feel comfortable during intercourse and avoid being too rough
If you experience bleeding related to hormonal birth control, talk to your doctor about other options
Maintain good vaginal health by having regular gynaecological examinations and managing any underlying conditions, such as fibroids or endometriosis
FAQ
Is bleeding after sex serious?
Occasional light bleeding after sex is relatively common and is often caused by minor issues such as vaginal dryness or hormonal changes. However, it's not normal and should be assessed by a healthcare professional, particularly if it keeps happening.
What if I experience pain or discomfort along with bleeding?
Bleeding accompanied by pain may suggest an infection, such as endometriosis, fibroids, or cervical irritation. Seek medical attention immediately if you experience severe pain, heavy bleeding, or a fever.
Is it safe to have sex again before seeing a doctor?
If the bleeding is light and quickly stops without any other symptoms, it is generally safe to have intercourse again. However, if the bleeding is heavy or painful, or if it happens repeatedly, you should avoid sexual intercourse until you've consulted a doctor.
Can bleeding during sex be related to my menstrual cycle?
Bleeding after sex is different from ovulation spotting or menstrual bleeding. However, if you have sexual intercourse close to the start or end of your period, it can be difficult to tell the difference. If you are uncertain, you can consider tracking when the bleeding occurs in relation to your cycle.
Can hormonal birth control cause bleeding during sex?
Yes. Hormonal birth control can cause breakthrough bleeding, which is irregular spotting that occurs between periods. This issue may happen after intercourse, but it isn't necessarily caused by it. Some hormonal contraceptives can also thin the vaginal lining, making it more likely to bleed during intercourse, particularly during the initial months of use.
Does postcoital bleeding affect fertility?
In most cases, postcoital bleeding itself does not affect fertility. However, if left untreated, some underlying causes, such as infections, endometriosis or cervical abnormalities, can impact your fertility. If you are trying to conceive and experience bleeding after sex, you should consult an obstetrician or gynaecologist (O&G).
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice, schedule an appointment at Thomson Women’s Clinic.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
