Testing positive for HPV can bring up a lot of questions and concerns, especially if you're already worried about cervical cancer. The good news is that most HPV infections never cause serious problems and will clear on their own within one to two years.
The real problems arise mainly when certain high-risk types of HPV stay in the body for a long time, gradually causing changes in your cervical cells. Knowing how this process happens – and how regular screening can detect these changes early – can help you feel more reassured and give you the confidence needed to take control of your cervical health.
What is HPV and why does it matter?
Human papillomavirus (HPV) is a group of more than 200 related viruses that can infect your skin and mucous membranes.
The virus spreads through intimate skin-to-skin contact during vaginal, anal, or oral sexual activity. One thing that makes HPV tricky is that it often doesn't cause any symptoms, so most people might not even notice that they’ve already been infected until they’ve done a screening test.
Fortunately, most HPV strains are harmless and won't cause any health problems. Some low-risk types can cause genital warts, which may be uncomfortable but aren't dangerous. The real problem comes from high-risk HPV types, which can lead to issues such as cervical cancer if they persist in your body for many years.
Knowing a few key facts about HPV can help put things into perspective:
HPV is very common:
Almost all sexually active people will get HPV at some point in their lives. This isn't about your choices – it simply reflects how widespread the virus is.
Your immune system usually clears it:
In most cases, your body clears HPV naturally within one to two years without any treatment needed.
Persistent infections need attention:
When high-risk HPV stays in your body for many years, it can interfere with your cervix cells’ growth and precancerous changes can develop.
Cervical cancer is one of the most preventable cancers because it develops so slowly. With regular Pap smears and HPV tests, you can often catch abnormal cell changes years before they could turn into cancer. When detected early, these changes can be treated with simple, effective procedures before they progress – giving you the best possible outcome.
How does HPV cause cervical cancer?
.png?branch=production)
HPV doesn't directly cause cancer the moment it enters your body. Instead, it's a gradual process that happens over many years.
High-risk HPV types and their role
Not all HPV types carry the same risk. Out of more than 200 HPV strains, about 14 are classified as high-risk for cervical cancer.
HPV 16 and 18 are the most concerning. These two types alone cause the majority of all cervical cancer cases worldwide. They're particularly persistent, meaning your body has a harder time clearing them.
Other high-risk types include HPV 31, 33, 45, 52, and 58. While these can also lead to cervical cancer, they're less common than types 16 and 18.
What makes these types "high-risk" is their ability to disrupt your cells' natural repair mechanisms. When this happens repeatedly over many years, normal cells can start turning cancerous and transform into abnormal cells.
The process from HPV infection to cervical cancer
The journey from HPV infection to cervical cancer happens in stages, which is why regular screening is so effective at catching changes early. The progression usually looks like this:
Stage 1 – Initial infection:
When high-risk HPV enters your cervix, your immune system usually clears it within one to two years. However, in some cases, the virus persists.
Stage 2 – Persistent infection (years 2-5):
If HPV remains in your body, it begins to affect your cervical cells' normal growth patterns, which can lead to changes over time.
Stage 3 – Precancerous changes (years 5-10):
Abnormal cells start to appear on your cervix surface. These are called cervical intraepithelial neoplasia (CIN) or dysplasia. At this stage, the changes are still not cancer and can be treated effectively.
Stage 4 – Progression to cancer (10-20+ years):
If precancerous cells go undetected and untreated, they can eventually develop into cervical cancer.
The slow progression from HPV infection to cancer works in your favour. It gives you multiple opportunities over many years to detect and treat any changes through regular screening, which is why keeping up with your cervical screening appointments matters.
If you're concerned about a persistent HPV infection or haven't had regular screening in several years, schedule an appointment with Thomson Medical. Our doctors can examine your cervical health and explain what steps to take next.
Risk factors that increase your chances of cervical cancer
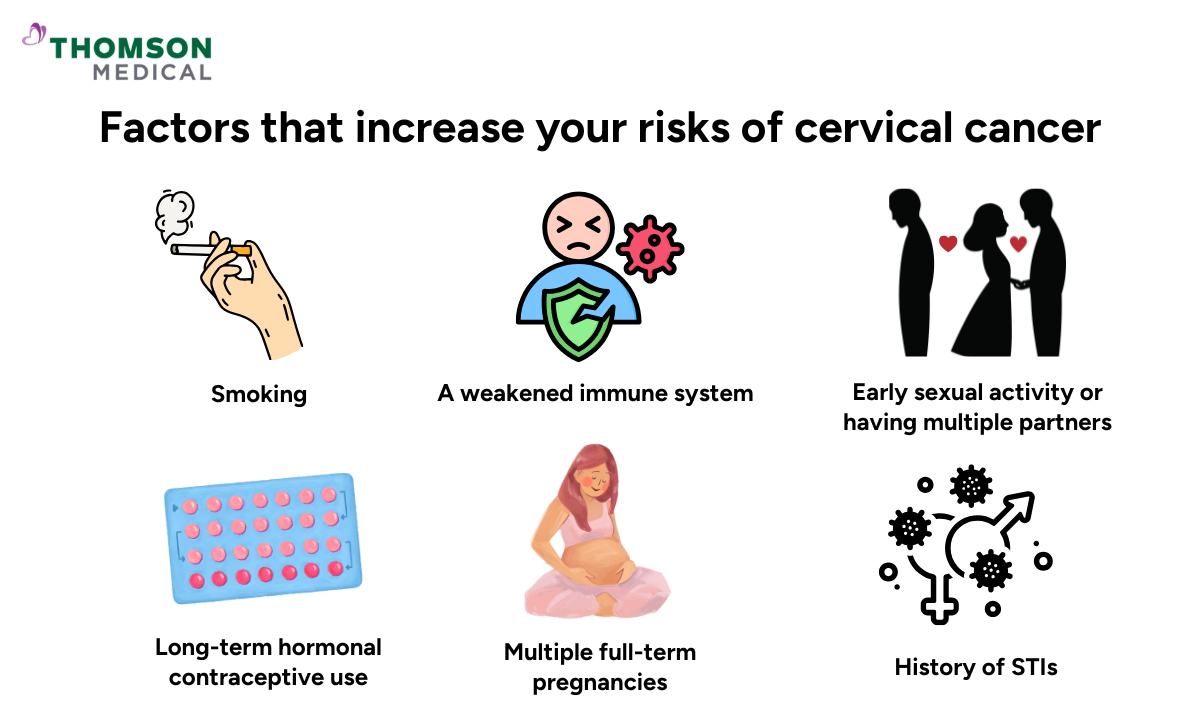
While anyone with a cervix can get HPV, certain factors can make it more likely for a high-risk infection to persist and develop into precancerous changes. Knowing these risk factors can help you take active steps to protect yourself:
Smoking:
Tobacco use makes it harder for your body to clear HPV infections naturally. Women who smoke are about twice as likely to develop cervical cancer compared to non-smokers.
A weakened immune system:
Your body may struggle to fight off persistent HPV infections if you have HIV, take immunosuppressant medications, or have other conditions that affect how your immune system works.
Early sexual activity or having multiple partners:
Starting sexual activity at a younger age or having multiple sexual partners increases your exposure to HPV, simply because the virus spreads so easily through skin-to-skin contact.
Long-term hormonal contraceptive use:
Using birth control pills for five years or more may slightly increase cervical cancer risk in women with HPV, though the reasons aren't fully clear.
The benefits of contraception often outweigh this risk, so it is recommended to discuss your options with your doctor rather than stopping on your own.
History of sexually transmitted infections:
If you have had other sexually transmitted infections (STIs), particularly chlamydia or herpes, it can increase inflammation in your cervix and make it easier for HPV to cause cell changes.
Multiple full-term pregnancies:
Women who have had three or more full-term pregnancies (ones that last 39 to 40 weeks) have a higher risk, possibly due to hormonal changes and how pregnancy affects the immune system.
It’s important to remember that just having any of these factors doesn't mean you're guaranteed to develop cervical cancer. These factors simply make it easier for a persistent HPV infection to linger. Regular screening remains your most powerful tool for protection.
If any of these risk factors apply to you or you're unsure how they might affect your cervical health, schedule an appointment with Thomson Medical. Our doctors can assess your specific situation and recommend a screening schedule that's right for you.
Prevention and early detection for cervical cancer
Two key approaches that help protect against HPV-related cervical cancer are vaccination and regular screening. Using both together provides you with thorough protection, significantly reducing your risk of developing cervical cancer and giving you peace of mind about your cervical health.
HPV vaccination
.png?branch=production)
HPV vaccines protect against the high-risk strains most commonly linked to cervical cancer, particularly types 16 and 18. The vaccine works best when given before exposure to HPV, which is why it's recommended for young people aged 9 to 14. That said, you can still benefit from it if you're up to age 26 or even 45.
Even if you've already been exposed to HPV, the vaccine can still protect you against other high-risk types you haven't encountered.
One thing to keep in mind is that the vaccine doesn't cover all HPV types that can cause cancer. This is why vaccination and regular screening work hand in hand. Both are important parts of looking after your cervical health.
Regular screening
As precancerous changes develop gradually over many years without symptoms, regular screening allows you to identify and address any changes early. Two screening tests that help detect cervical abnormalities are the Pap smear and the HPV test:
Pap smear (Pap test):
Your doctor collects cells from your cervix to check for abnormal changes. The sample is examined under a microscope to identify precancerous changes.
Doctors generally recommend Pap smears every three years if you are between 21 and 29.
HPV test:
The HPV test identifies high-risk HPV types in your cervical cells.
This test is usually recommended if you are 30 or above, either on its own every five years or alongside a Pap smear.
A positive HPV result is common and doesn't mean you have cancer. Many HPV infections clear naturally, which is why your doctor may recommend follow-up screening.
Co-testing:
Co-testing involves both tests at the same appointment. If you are between 30 and 65, this approach every five years provides comprehensive screening.
When both tests show negative results, the likelihood of you developing cervical cancer within the next several years is significantly reduced.
Both tests are brief, usually completed within a few minutes during a routine gynaecological examination. While you may experience slight discomfort, the procedure is generally not painful.
Think of vaccination and screening as two layers of protection working together for you. Vaccination reduces your risk of getting high-risk HPV in the first place, while screening catches any cell changes early if an infection does occur. When you use both, you're taking active steps to protect your cervical health and reduce your cervical cancer risk as much as possible.
Cervical cancer specialists in Singapore
Loading...
FAQ
Can HPV infections clear on their own without causing cancer?
Yes. Most HPV infections clear naturally within one to two years as your immune system fights off the virus. Only a small percentage of infections persist long enough to cause cell changes that could lead to cancer.
How long does it take for HPV to develop into cervical cancer?
It usually takes 10 to 20 years for a persistent high-risk HPV infection to progress to cervical cancer, though it can happen faster in people with weakened immune systems. This slow progression is why regular screening is so effective at catching changes early.
Does testing positive for HPV mean I will get cancer?
Testing positive for HPV is extremely common and doesn't mean you are guaranteed to develop cancer. Most HPV infections clear on their own, and even persistent infections can be monitored and treated before they ever become cancer.
Can I still get HPV if I've been vaccinated?
Yes, but your risk is much lower. The vaccine protects against the most dangerous HPV types but not all of them. You can still be exposed to types not covered by the vaccine, which is why screening remains important even after vaccination.
What are the early warning signs of cervical cancer?
Precancerous changes and early cervical cancer rarely cause symptoms, which is why screening is so important. If symptoms do appear, they may include abnormal vaginal bleeding, unusual discharge, or pelvic pain. If you notice any of these, discuss them with your doctor.
What should I do if my HPV test comes back positive?
Try not to panic. Follow your doctor's recommendations, which normally include repeat testing or a colposcopy to check for cell changes. Most positive HPV tests don't require immediate treatment – just monitoring to make sure the infection clears naturally.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
Citations
Human papillomavirus (HPV). (n.d.). https://www.who.int/teams/health-product-policy-and-standards/standards-and-specifications/norms-and-standards/vaccine-standardization/human-papillomavirus
World Health Organization: WHO & World Health Organization: WHO. (2024, March 5). Human papillomavirus and cancer. https://www.who.int/news-room/fact-sheets/detail/human-papilloma-virus-and-cancer
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
.png%3Fbranch%3Dprod&w=3840&q=75)