Whether you're just starting to learn about your body, planning a pregnancy, or looking to protect your sexual health, understanding how your body works is the first step. Let's take a look at the key things you should know to help you feel more confident and in control of your sexual and reproductive health.
What is sexual and reproductive health for women?

Sexual and reproductive health concerns your physical, mental, and social well-being connected to your reproductive system. It includes:
Understanding your menstrual cycle and reproductive organs
Preventing and treating sexually transmitted infections (STIs)
Access to contraception and family planning
Safe pregnancy and childbirth
Managing reproductive health conditions
More importantly, it’s also about getting the right care and support without fear, shame, or judgement.
Adolescent sexual health
Adolescents are likely to face many health and social challenges. If they start becoming sexually active without having enough knowledge about how to protect themselves, they are at higher risks of unwanted pregnancy, unsafe termination of pregnancy (abortion), and STIs, including HIV/AIDS.
These issues can have a significant impact on their health and wellbeing, with potentially life-threatening complications. Young women who become pregnant during their teenage years are also at higher risk of complications, such as anaemia, postpartum bleeding, and depression.
Maternal sexual health
Maternal sexual health refers to taking care of your overall well-being during pregnancy, childbirth, and the postbirth period.
Key aspects of maternal health include:
Access to integrated maternal care:
This includes prenatal care, safe delivery services, and postbirth support, along with access to information and services related to contraception, STIs, and family planning.
Addressing specific health challenges:
STIs:
Preventing and treating STIs are crucial because without treatments, they can lead to severe complications, including infertility, pelvic inflammatory disease, and pregnancy-related issues.
Pelvic floor health:
According to the National Institutes of Health (NIH), exercises like pelvic floor muscle training can improve strength, which is beneficial for sexual function and recovery after childbirth.
Postbirth recovery and sexual health:
Physiological recovery:
The body needs time to heal after childbirth. However, the recovery varies for each individual, with many women feeling well again by about 8 weeks after delivery.
Mental and emotional support:
Sexual health counselling can be useful for improving sexual satisfaction after childbirth. It’s normal if you have questions and concerns during this time.
Partner communication:
Open communication with your partner is essential for maintaining a healthy sexual relationship after childbirth.
Your period cycle

A period cycle, or menstrual cycle, is a series of hormonal changes that prepare the body for a possible pregnancy. It starts on the first day of your period and ends the day before your next period begins. Although most cycles last around 28 days, they can vary from person to person. Your cycle can range from 21 to 35 days, and that’s normal.
Your cycle includes four phases:
Menstruation:
This phase happens because you didn’t get pregnant in the previous cycle, so your body sheds the lining of your uterus (womb). Your period usually lasts 3 to 7 days. However, it's different for everyone.
Follicular phase:
This phase starts on the first day of your period and continues as it ends. During this time, hormones will stimulate the ovaries to produce follicles containing immature eggs.
As the follicles mature, they release oestrogen, which thickens the uterine lining in preparation for pregnancy.
Ovulation:
Around the middle of your menstrual cycle, a surge in the level of the luteinising hormone (LH) triggers ovulation, which is the release of a mature egg from the follicle in the ovary.
The egg then travels down the fallopian tube, where it can meet sperm and be fertilised. Ovulation typically happens 10 to 16 days before the next period starts.
Luteal phase:
After ovulation, the empty follicle changes into a structure (corpus luteum) that produces progesterone to maintain the lining of the uterus.
However, if the egg isn’t fertilised, the corpus luteum breaks down and causes a drop in oestrogen and progesterone levels. When these hormone levels fall, the uterine lining starts to break down, leading to the start of the next period.
Knowing your cycle can help you know what’s normal for your body and recognise if something might be off. Every woman has a unique period cycle, so don’t worry if you experience it longer than others. What matters is knowing what’s normal for you.
Fertility and pregnancy
Fertility refers to your ability to conceive a baby, and pregnancy occurs when a sperm successfully fertilises an egg. Knowing how your reproductive system works, can help you plan for a healthy pregnancy.
Timing is important to increase the chances of conception. This means you should have intercourse during the fertile window, which is the days leading up to and including ovulation.
Living a healthy lifestyle also helps. This involves eating a balanced diet, staying active with moderate exercise, and taking care of your overall well-being.
How to optimise for pregnancy
Time of intercourse:
The fertile window is when you’re most likely to get pregnant. This includes the five days before you ovulate, the day of ovulation, and the day after. An egg only lives for about 12 to 24 hours, while sperm can live for up to 5 days in the body.
Know your cycle:
Tracking your menstrual cycle helps you understand when ovulation typically occurs. If you have a 28-day cycle, ovulation is often around day 14, though everyone is different.
It’s also important to pay attention to your body. Changes in vaginal discharge, such as a clear, stretchy, egg-white-like consistency, can also indicate you are in your fertile window.
How to maintain a healthy lifestyle
Weight:
Being overweight or underweight can interfere with ovulation, so aiming for a healthy weight can support your fertility.
Exercise:
Regularly engaging in moderate activity is beneficial for your overall health. However, avoid doing overly strenuous activity.
Nutrition:
Focus on nutrient-dense foods and reduce processed foods, added sugars, and caffeine (especially if you have over 200mg per day).
Habits:
Smoking and drinking alcohol can negatively affect fertility and pregnancy outcomes. That’s why it’s best to maintain healthy habits and avoid these as much as possible.
Prenatal vitamins:
Consider starting a prenatal vitamin before you get pregnant. This vitamin often contains folic acid, which helps reduce the risk of neural tube abnormalities like spina bifida.
Stress management:
While stress alone is unlikely to prevent pregnancy, managing stress through activities like meditation or yoga is beneficial for both your mental and physical health along the journey.
Each woman's fertility journey is unique. If you've been trying to conceive without success, you can consult with our obstetrician and gynaecologist (O&G) specialists for personalised care and fertility guidance.
Once you're pregnant, regular antenatal care plays an important role in improving health outcomes for both you and your baby throughout your pregnancy.
Our gynaecologist
Loading...
Contraception and family planning
Family planning involves making informed decisions about if, when, and how many children you want to have. It's a fundamental part of reproductive health that puts you in control of your choices.
Contraception, on the other hand, is one key tool in family planning. The procedure allows women to prevent pregnancy when they're not ready to have a baby. Other aspects of family planning include fertility support, preconception care, and reproductive health education.
Both are fundamental to women's sexual and reproductive health. It gives you control over your reproductive choices so you can make decisions that are right for you and your family. There are several contraceptive methods, including:
Hormonal methods:
These work by using hormones to prevent pregnancy. The most common choice is the birth control pill, but you can also choose others, such as injections, implants, and patches.
Barrier methods:
These block sperm from reaching an egg. Options usually include male and female condoms, diaphragms, and cervical caps.
Intrauterine devices (IUDs):
IUDs are small devices that your doctor will place in the uterus. They have 2 types: hormonal IUDs or non-hormonal IUDs.
Permanent methods:
Sterilisation is a surgical procedure available for both men and women. It is a permanent form of contraception.
Emergency contraception:
You can use an emergency contraception after unprotected sex to prevent pregnancy. It works best when you take it as soon as possible.
Natural family planning:
This method involves tracking ovulation to identify your fertile days and avoid intercourse during these periods.
Choosing the right contraceptive methods is a personal decision. However, your doctor can help you find the one that works best for you and answer any questions you might have about this topic.
Whether you're planning a pregnancy or exploring contraception options, schedule an appointment with Thomson Medical for personalised care and support.
Sexually transmitted infections
Sexually transmitted infections (STIs) can have serious impacts on women’s health. They can cause problems such as infertility, chronic pelvic pain, and even certain types of cancer, including cervical cancer from Human Papillomavirus (HPV).
If left untreated, STIs can lead to serious complications, such as pelvic inflammatory disease (PID), pregnancy complications for the baby, and higher susceptibility to contracting HIV.
That’s why regular STI screening is crucial to help you detect infections early and prevent these long-term health problems.
Major health consequences women can face:
Pelvic inflammatory disease (PID):
Chlamydia and gonorrhoea can spread to the uterus and fallopian tubes. This causes a condition called PID, which can lead to difficulty in getting pregnant in the future.
Cancers:
Certain types of HPV can lead to cervical cancer, vaginal cancer, vulvar cancer, and throat cancer.
Infertility:
Untreated infections can damage your reproductive organs and result in permanent infertility.
Pregnancy complications:
If you have untreated STIs during pregnancy, it can affect both you and your baby. Risks can include premature birth, low birth weight, and life-threatening conditions for the newborn.
Increased risk of HIV:
Certain STIs, such as herpes, gonorrhoea, and syphilis, increase your risk of contracting HIV if you’re exposed to the virus.
Chronic pain:
Some untreated infections can result in chronic pelvic pain.
Other issues:
STIs can also cause complications like arthritis, eye inflammation, and even heart disease.
STIs are treatable, but many of them don’t show clear symptoms, especially in the early stages. If you’re sexually active, it’s better to have regular testing. It’s a normal part of taking care of your health, so there’s nothing to feel embarrassed about. Protecting yourself also means protecting your partners and your future health.
Common reproductive health issues
Women can experience various reproductive health concerns. Some of the most common issues include:
Menstrual cycle disorders
Heavy or irregular bleeding:
Bleeding that is heavy, lasts longer than usual, or happens outside of normal periods.
Amenorrhoea:
Premenstrual syndrome (PMS) and PMDD:
PMS causes mood changes and physical symptoms before your period starts. PMDD is more severe and can affect your daily life.
Structural and hormonal issues
These are noncancerous tumours that develop in or on your uterus. They can cause heavy bleeding, pelvic pain, and pressure.
Endometriosis:
This happens when tissue similar to the uterine lining grows outside the uterus. The condition usually causes pain.
Polycystic ovary syndrome (PCOS):
A hormonal disorder causing cysts on the ovaries, irregular periods, and high levels of male hormones.
Infertility and pregnancy
Infertility:
It refers to the difficulty of conceiving after trying for a year.
Problems during pregnancy:
Various complications can occur during your pregnancy that need proper medical care.
Infections and other conditions
Sexually transmitted infections (STIs):
These infections, caused by bacteria, parasites, or viruses, may lead to infertility or other serious health problems for women if untreated.
Interstitial cystitis (IC):
This is a chronic bladder condition that causes pelvic pain and pressure, along with frequent or urgent urination.
Many of these conditions are treatable, especially when you detect them early. If you notice symptoms like unusual pain, heavy bleeding, or irregular periods, or anything else that doesn’t feel normal for your body, consult your doctor to receive guidance.
Treatments for female sexual dysfunction
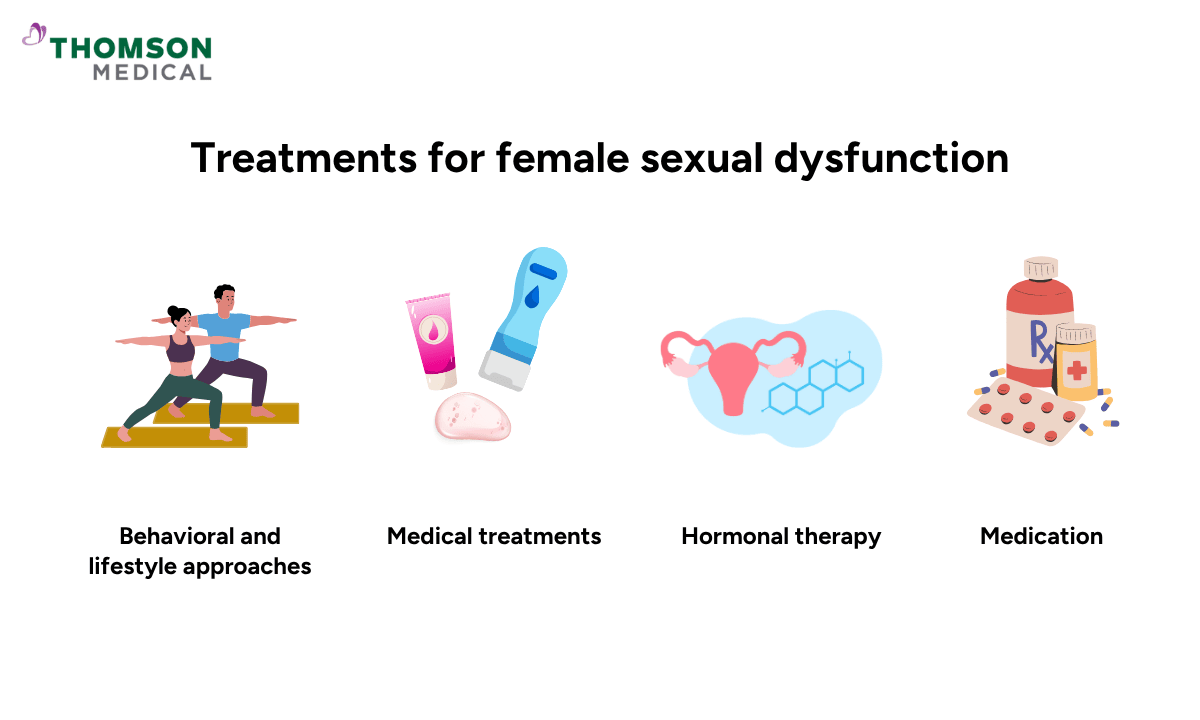
Treatments for female sexual dysfunction (FSD) are multifaceted and can include therapy, lifestyle changes, and medication. Common approaches involve communication with your partner, counselling or sex therapy, and managing underlying health factors.
In some cases, medical options may include vaginal lubricants and moisturisers, hormonal therapies or specific medications may also be recommended depending on the cause. The best treatment will depend on what’s causing your symptoms, so it’s personalised to your specific situation.
Treatments that your doctor can suggest to you:
Behavioral and lifestyle approaches
Open communication:
Open and honest communication with your partners about your needs and desires can make a big difference in your sexual life.
Counselling:
Speaking with a therapist on your own or as a couple can help address psychological, relational, and sociocultural factors contributing to FSD.
Education:
Learning about sexual function can be a valuable part of treatment.
Stay sexually active:
Regular sexual activity can help maintain sexual function.
Lifestyle changes:
Living a healthy lifestyle, such as eating well, exercising regularly, and getting enough sleep, can support your overall health.
Medical treatments
Lubricants and moisturisers:
While vaginal lubricants can help reduce discomfort or pain during intercourse, vaginal moisturisers can also be beneficial if you experience vaginal dryness.
Hormonal therapy
Oestrogen:
If you’re going through or past menopause, oestrogen therapy can be effective for vaginal pain and dryness
Testosterone:
Your doctor may suggest that you use testosterone therapy to improve sexual function after menopause, though long-term safety and effectiveness data are still being researched.
Medications
For low libido:
Specific medications like bremelanotide and flibanserin are available to treat low sex desire, particularly in premenopausal women.
For antidepressant side effects:
Your doctor may add bupropion to your treatment to counteract sexual side effects caused by certain antidepressants.
Other options:
Medications like PDE5 inhibitors (e.g., sildenafil) may be considered in some cases. However, research on how effective these medications are for women is still limited.
Addressing female sexual dysfunction is not just about treatment. It's also about understanding female sexuality and helping you feel more confident, comfortable, and connected to your bodies.
If you want to take a proactive approach to your sexual and reproductive health, schedule an appointment with Thomson Medical. Our specialists can help with further testing, diagnosis, and supportive care in a judgement-free environment.
FAQ
How late can a period be before pregnancy becomes an option?
If your regular cycle is more than 7 days late, it could be a sign of pregnancy. It’s a good time to take a home pregnancy test.
It’s totally normal if your period is late for a few days. Things like stress or weight change can delay your period. However, a period over a week late is a strong indicator of pregnancy, and taking a test is a reliable way for you to have an answer.
How can I track my ovulation?
You can track ovulation by using:
- The calendar method for regular cycles
- Ovulation predictor kits (OPKs) to detect the LH surge
- Monitoring cervical mucus for egg-white-like consistency
- Tracking your basal body temperature (BBT) for a slight rise after ovulation has occurred.
Many women find that combining these methods, such as using OPKs along with tracking cervical mucus, often provides the most reliable results.
What are the different types of birth control, and how effective are they?
Birth control methods include:
- Long-acting reversible contraceptives (LARCs):
- IUDs and implants are over 99% effective
- Hormonal options:
- Birth control pills, patches, rings, and shots range from 93% to 99% effective
- Barrier methods:
- Condoms, diaphragms, and cervical caps are 79-98% effective.
Other options include permanent sterilisation (over 99% effectiveness) and natural methods, which are generally less effective.
Effectiveness varies significantly from person to person, depending on the method you use and how consistently you use it.
How can I protect myself from STIs?
There are several ways that can help you protect yourself from STIs. They include:
- Practise safe sex:
- Always using condoms consistently and correctly
- Get vaccinated:
- Vaccines for STIs, especially HPV and hepatitis B, can protect you from serious health problems
- Limit your number of sexual partners:
- This can reduce your exposure risk
What are the most common female sexual and reproductive health issues?
Women can experience various sexual and reproductive health concerns, including:
- Menstrual cycle disorders like PMS and heavy bleeding
- Infections such as UTIs and Pelvic Inflammatory Disease (PID)
- Hormonal conditions like PCOS
- Structural problems like uterine fibroids and endometriosis
- Breast conditions like fibrocystic changes
- Issues related to pregnancy and childbirth
What are the 5 P's of sexual health?
The 5 P’s of sexual health are Partners, Practices, Protection from STIs, Past history of STIs, and Pregnancy intention. They are key areas to understand when it comes to your sexual well-being.
They will help your doctor learn more about your needs and experience so your doctor can offer the right care and support your sexual and reproductive health.
The information provided is intended for general guidance only and should not be considered medical advice. For personalised recommendations and tailored advice based on your unique conditions, please consult a specialist at Thomson Medical. Request an appointment with Thomson Medical today.
For more information, contact us:
Thomson Specialists (Women's Health)
Thomson Women's Clinic (TWC)
- Novena:
6592 6686 (Call), 8611 8986 (WA) - Bukit Batok:
6569 0668 (Call), 8686 3525 (WA) - Choa Chu Kang:
6893 1227 (Call), 8282 1796 (WA) Jurong:
6262 8588 (Call), 6262 8588 (WA)- Katong (female doctor):
6970 2272 (Call), 8611 9020 (WA) - Punggol:
6243 6843 (Call), 8811 0328 (WA) - Sembawang: 6753 5228
- Sengkang: 6388 8125
- Serangoon (female doctor): 6382 3313
- Tampines: 6857 6266
- Tiong Bahru: 6276 1525
